
80 The Open Health Services and Policy Journal, 2010, 3, 80-100
Open Access
1874-9240/10 2010 Bentham Open
Shelter from the Storm: Trauma-Informed Care in Homelessness Services
Settings
Elizabeth K. Hopper
*,1
, Ellen L. Bassuk
2,3
, and Jeffrey Olivet
4
1
The Trauma Center at JRI 1269 Beacon Street Brookline, MA 02446, USA
2
The National Center on Family Homelessness, 181 Wells Avenue, Newton, MA 02459, USA
3
Department of Psychiatry, Harvard Medical School, USA
4
Centre for Social Innovation 215 Spadina Avenue, Suite 120 Toronto, Ontario M5T 2C7, Canada
Abstract: It is reasonable to assume that individuals and families who are homeless have been exposed to trauma.
Research has shown that individuals who are homeless are likely to have experienced some form of previous trauma;
homelessness itself can be viewed as a traumatic experience; and being homeless increases the risk of further
victimization and retraumatization. Historically, homeless service settings have provided care to traumatized people
without directly acknowledging or addressing the impact of trauma. As the field advances, providers in homeless service
settings are beginning to realize the opportunity that they have to not only respond to the immediate crisis of
homelessness, but to also contribute to the longer-term healing of these individuals. Trauma-Informed Care (TIC) offers a
framework for providing services to traumatized individuals within a variety of service settings, including homelessness
service settings. Although many providers have an emerging awareness of the potential importance of TIC in homeless
services, the meaning of TIC remains murky, and the mechanisms for systems change using this framework are poorly
defined. This paper explores the evidence base for TIC within homelessness service settings, including a review of
quantitative and qualitative studies and other supporting literature. The authors clarify the definition of Trauma-Informed
Care, discuss what is known about TIC based on an extensive literature review, review case examples of programs
implementing TIC, and discuss implications for practice, programming, policy, and research.
Keywords: Homelessness, trauma, trauma-informed, systems change.
INTRODUCTION
Trauma-Informed Care: A Paradigm Shift for Homeless
Services
“Homelessness deprives individuals of…basic
needs, exposing them to risky, unpredictable
environments. In short, homelessness is more
than the absence of physical shelter, it is a
stress-filled, dehumanizing, dangerous circums-
tance in which individuals are at high risk of
being witness to or victims of a wide range of
violent events” [1].
Homelessness is a traumatic experience. Individuals and
families experiencing homelessness are under constant
stress, unsure of whether they will be able to sleep in a safe
environment or obtain a decent meal. They often lack a
stable home and also the financial resources, life skills, and
social supports to change their circumstances. In addition to
the experience of being homeless, an overwhelming
percentage of homeless individuals, families, and children
have been exposed to additional forms of trauma, including:
neglect, psychological abuse, physical abuse, and sexual abuse
during childhood; community violence; combat-related
*Address correspondence to this author at the Trauma Center at JRI 1269,
Beacon Street Brookline, MA 02446, USA; Tel: (617) 232-1303, Ext.
211; E-mail: ehopper@jri.org
trauma; domestic violence; accidents; and disasters. Trauma
is widespread and affects people of every gender, age, race,
sexual orientation, and background within homeless service
settings.
Early developmental trauma—including child abuse,
neglect, and disrupted attachment—provides a subtext for
the narrative of many people’s pathways to homelessness
[2]. Violence continues into adulthood for many people, with
abuse such as domestic violence often precipitating
homelessness [3-5], and with homelessness leaving people
vulnerable to further victimization. The impact of traumatic
stress often makes it difficult for people experiencing
homelessness to cope with the innumerable obstacles they
face in the process of exiting homelessness [6], and the
victimization associated with repeated episodes of
homelessness. Research has found that people who
experienced repeated homelessness were more likely than
people with a single episode of homelessness to have been
abused, often during childhood [6].
Trauma refers to an experience that creates a sense of
fear, helplessness, or horror, and overwhelms a person’s
resources for coping. The impact of traumatic stress can be
devastating and long-lasting, interfering with a person’s
sense of safety, ability to self-regulate, sense of self,
perception of control and self-efficacy, and interpersonal
relationships. Some people have minimal symptoms after
trauma exposure or recover quickly, while others may
Trauma-Informed Care in Homelessness The Open Health Services and Policy Journal, 2010, Volume 3 81
develop more significant and longer-lasting problems such
as Posttraumatic Stress Disorder (PTSD) and Complex
Trauma.
Trauma reactions are not the only psychiatric issue facing
people who are homeless; many people experiencing
homelessness also suffer from depression, substance abuse [7-
10], and severe mental illness [8, 10]. These issues leave
individuals even more vulnerable to revictimization [11],
interfere with their ability to work, impair their social networks
[8], and further complicate their service needs.
These findings suggest that we will be unable to solve the
issue of homelessness without addressing the underlying trauma
that is so intricately interwoven with the experience of
homelessness. Those working in homeless services have the
opportunity to reach many trauma survivors who are otherwise
overlooked. Providers in these settings address the immediate
crisis by offering food, shelter, and clothing; but they can also
contribute to longer-lasting changes by helping an individual or
family develop supportive connections in the community and
begin to heal from past traumas. Despite this fact, few programs
serving homeless individuals and families directly address the
specialized needs of trauma survivors. Homeless services have a
long history of serving trauma survivors, without being aware
of or addressing the impact of traumatic stress [12].
Overwhelmed by the daily needs of their clients, providers in
these settings often have few resources to address issues of
long-term recovery.
With increasing recognition of the pervasiveness of
traumatic stress among people experiencing homelessness,
awareness is growing of the importance of creating Trauma-
Informed Care within homeless services settings. Trauma-
Informed Care (TIC) involves “understanding, anticipating, and
responding to the issues, expectations, and special needs that a
person who has been victimized may have in a particular setting
or service. At a minimum, trauma-informed services endeavor
to do no harm—to avoid retraumatizing or blaming [clients] for
their efforts to manage their traumatic reactions” [13].
Implementing TIC requires a philosophical and cultural shift
within an agency, with an organizational commitment to
understanding traumatic stress and to developing strategies for
responding to the complex needs of survivors.
Despite its importance, the implementation of TIC within
homelessness service settings is still in its infancy. Currently,
the nature of TIC remains ill-defined. Strategies for
implementation are obscure, few program models exist, and
there is limited communication and collaboration among
programs implementing TIC. The descriptive and research
literature in this area is sparse, with only a handful of studies
examining the nature and impact of TIC. More clarification is
needed about what exactly defines TIC, what changes should be
made within systems wishing to offer TIC, and how these
changes should be implemented.
The purpose of this paper is to review the evidence base that
supports the use of TIC for individuals and families
experiencing homelessness. In this review, we have attempted
to:
• Establish a consensus-based definition of TIC
• Discuss what is known about TIC based on our literature
review
• Describe models and case examples of what is being
done in the field to implement TIC within homeless
service settings
We conclude by summarizing implications of our current
state of knowledge for practice, programming, policy, and
research and by highlighting next steps for developing
evidence-based, trauma-informed homeless services.
What is Trauma-Informed Care (TIC)?
What is meant by TIC? Although there is agreement that
“trauma-informed” refers generally to a philosophical/ cultural
stance that integrates awareness and understanding of trauma,
there is no consensus on a definition that clearly explains the
nature of TIC.
TIC supports the delivery of Trauma-Specific Services
(TSS). TSS refers to interventions that are designed to directly
address the impact of trauma, with the goals of decreasing
symptoms and facilitating recovery. TSS differs from TIC, in
that TSS are specific treatments for mental disorders resulting
from trauma exposure, while TIC is an overarching framework
that emphasizes the impact of trauma and that guides the
general organization and behavior of an entire system. TSS may
be offered within a trauma-informed program or as stand-alone
services [12].
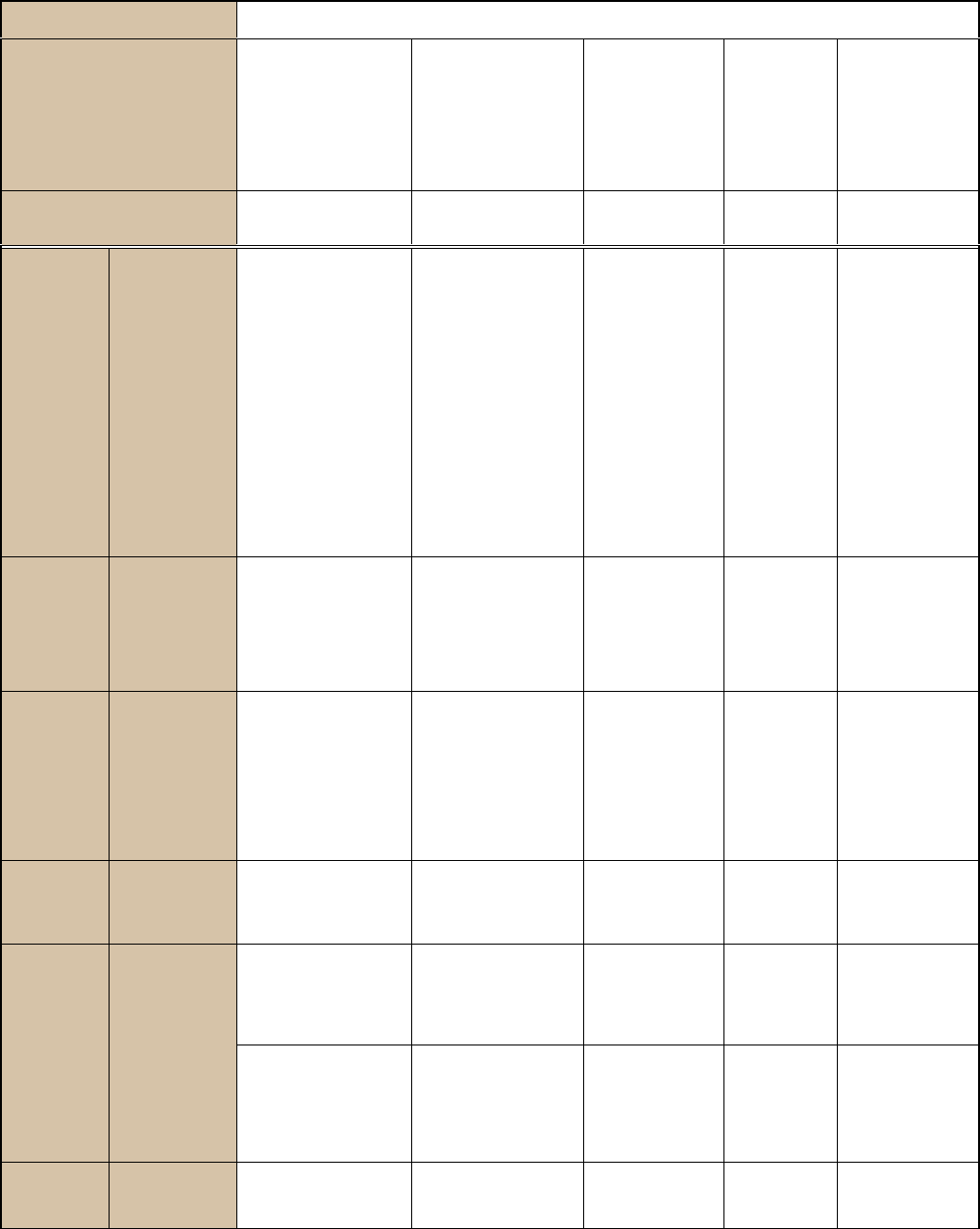
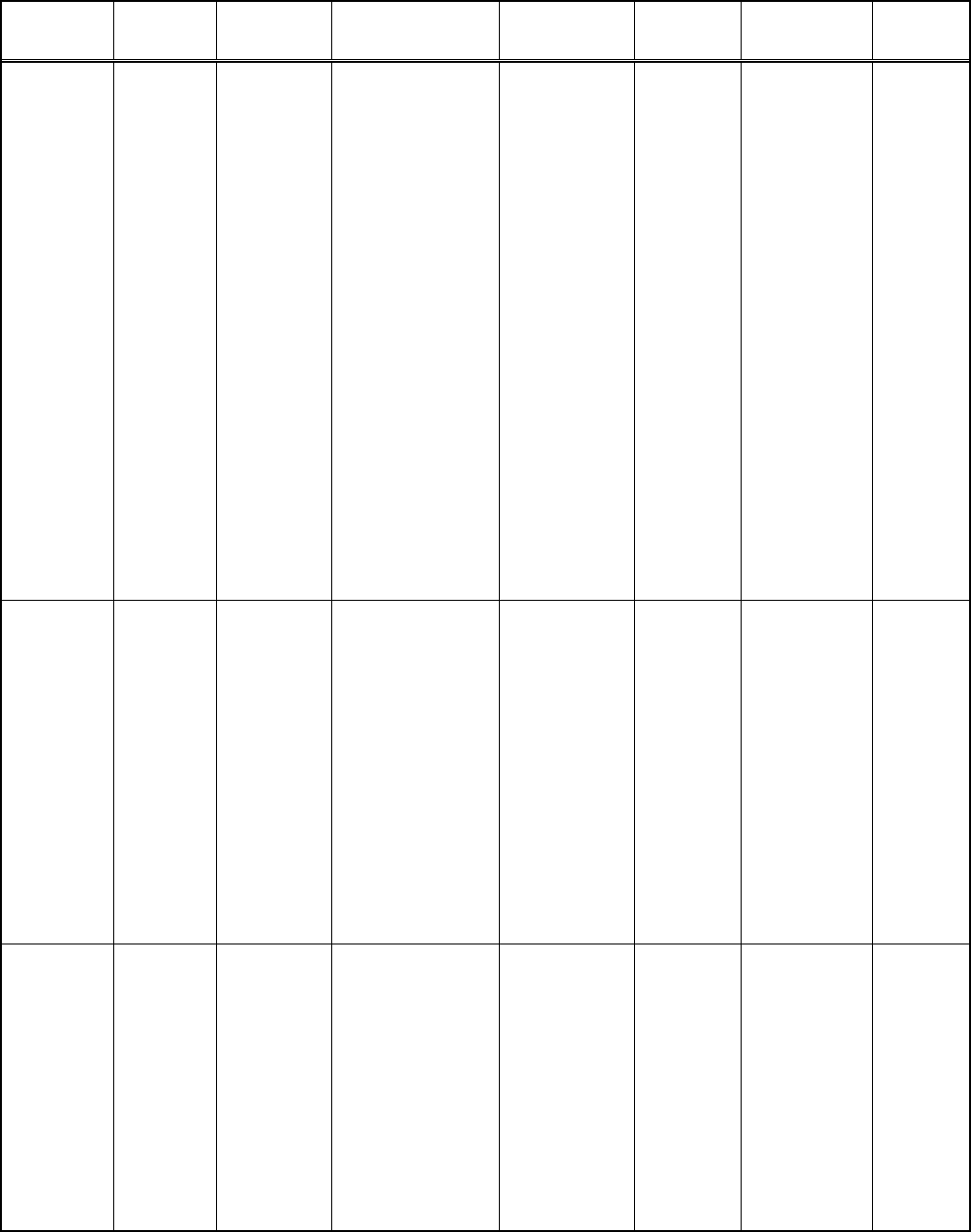
Based on the literature review, we summarized the basic
principles of TIC proposed by various workgroups,
organizations, expert panels, and researchers. (see Table 1).
Each of these sources posited a unique definition of TIC. We
identified and highlighted common cross-cutting themes and
then synthesized them into a single definition. Themes include:
• Trauma awareness: Trauma-informed service
providers incorporate an understanding of trauma into
their work. This may involve altering staff perspectives,
with providers understanding how various symptoms
and behaviors represent adaptations to traumatic
experiences. Staff training, consultation, and supervision
are important aspects of organizational change towards
TIC and organizational practices should be modified to
incorporate awareness of the potentially devastating
impact of trauma. For example, agencies may implement
routine screening for histories of traumatic exposure,
may conduct routine assessments of safety, and may
develop strategies for increasing access to trauma-
specific services. Dealing with vicarious trauma and
self-care is also an essential ingredient of trauma-
informed services. Many providers have experienced
trauma themselves and may be triggered by client
responses and behaviors.
• Emphasis on safety:
Because trauma survivors often
feel unsafe and may actually be in danger (e.g., victims
of domestic violence), TIC works towards building
physical and emotional safety for consumers and
providers. Precautions should be taken to ensure the
physical safety of all residents. In addition, the
organization should be aware of potential triggers for
consumers and strive to avoid retraumatization. Because
interpersonal trauma often involves boundary violations
and abuse of power, systems that are aware of trauma
dynamics should establish clear roles and boundaries
that are an outgrowth of collaborative decision-making.
82 The Open Health Services and Policy Journal, 2010, Volume 3 Hopper et al.
Privacy, confidentiality, and mutual respect are also
important aspects of developing an emotionally safe
atmosphere. Additionally, cultural differences and
diversity (e.g., gender, ethnicity, sexual orientation) must
be addressed and respected within trauma-informed
settings.
• Opportunities to rebuild control: Because control is
often taken away in traumatic situations, and because
homelessness itself is disempowering, trauma-
informed homeless services emphasize the
importance of choice for consumers. They create
predictable environments that allow consumers to re-
build a sense of efficacy and personal control over
their lives. This includes involving consumers in the
design and evaluation of services.
• Strengths-based approach: Finally, TIC is
strengths-based, rather than deficit-oriented. These
service settings assist consumers to identify their own
strengths and develop coping skills. TIC service
settings are focused on the future and utilize skills-
building to further develop resiliency.
These principles form a standard for programs wishing to
develop TIC within homeless service settings. Based on
these combined principles, we developed a consensus-based
definition of TIC:
Consensus-Based Definition
“Trauma-Informed Care is a strengths-based
framework that is grounded in an understanding of
and responsiveness to the impact of trauma, that
emphasizes physical, psychological, and emotional
safety for both providers and survivors, and that
creates opportunities for survivors to rebuild a
sense of control and empowerment.”
Trauma-informed approaches are designed to respond to
the impact of trauma. The principles described above target
the specialized needs of trauma survivors and describe how
services can be delivered through the lens of trauma.
METHODS
This paper reviews the evidence base supporting the
effectiveness of TIC for people experiencing homelessness. To
date, most determinations of what constitutes evidence-based
practice have relied on outcome-based quantitative research.
However, this approach neglects qualitative analyses that
examine the nature and process of the intervention, as well as a
wealth of information that reflects what is occurring in practice.
In fact, corroborative evidence, including clinical wisdom about
“what works,” is often the starting point for developing both
qualitative and quantitative studies. In the homelessness field,
corroborative evidence may be the primary body of knowledge
we have about a particular intervention.
For this review, we utilized a comprehensive framework
tha
t was developed by the Homelessness Resource Center
(HRC) for assessing the level of evidence of an emerging,
promising or best practice [15]. The goal of this framework is
not to decide whether a practice qualifies as evidence-based, but
rather to synthesize all that we currently know about the
intervention. Thus, our review included peer-reviewed
quantitative and qualitative studies, as well as corroborative
literature (e.g., program evaluations and unpublished pilot
studies).
The literature on TIC is significantly greater in mental health
and substance use fields than within the homelessness field.
Thus, we also reviewed the current evidence base for trauma-
informed practices in these areas since there is a large overlap in
the difficulties faced by many individuals with mental
health/substance use issues and those in homeless service
settings. In fact, in the Women, Co-Occurring Disorders, and
Violence Study (WCDVS), a large multi-site study examining
trauma-informed services for women with co-occurring
disorders and trauma exposure, 70.4% of participants had been
homeless at some point in their lives [16]. We reviewed
evidence for trauma-informed services within all these settings,
applying this broader knowledge base to our understanding of
TIC within homeless service settings.
We conducted our literature review by searching two
databases, PsycInfo and Medline (PubMed), for peer-reviewed
articles published in major journals. In addition, we used the
Google search engine to locate web-based literature and
program information. Our search terms included: homeless,
homelessness, housing, shelters, trauma, trauma-informed,
PTSD, services, abuse, violence, domestic violence,
psychological, substance use, and mental health. We also
completed more specialized searches on unique populations
(using search terms such as youth, men, ethnicity, veterans),
authors of note (e.g., Harris, Fallot, Bassuk, and van der Kolk),
models (e.g., Attachment, Self-Regulation and Competency
[ARC] and Sanctuary), programs (e.g., Community
Connections, the STAR program, and the Community Trauma
Treatment Center for Runaway and Homeless Youth), and
research studies (e.g., the Women, Co-Occurring Disorders, and
Violence Study).
In addition to reviewing the literature, we contacted various
programs directly, by telephone or email, including: the Natio-
nal Center on Family Homelessness (Moses, Guarino); Home-
lessness Resource Center (Olivet); Community Connections
(Fallot); the Institute for Health and Recovery (Markoff &
Dargon-Hart); CT State Department of Mental Health and
Addiction Services (Leal); the Domestic Violence & Mental
Health Policy Initiative (Brashler, Hall); the Community
Trauma Treatment Center for Runaway and Homeless Youth
(Schneir); the Trauma Center at JRI/ Youth on Fire, developers
of Phoenix Rising (Spinazzola); Kinniburgh and Blaustein,
developers of ARC; Cincinnati Children's Hospital Medical
Center, developers of CARE (Pearl); University of Connecticut
Department of Psychology and the CT Department of Mental
Health and Addiction Services Research Division (Marra). Many
of these programs sent unpublished program evaluation reports,
manuals, or self-assessment tools, for inclusion in this review.
RESULTS
Organizational Needs Assessments: Do We Need
Trauma-Informed Care?
Needs assessments can be used to identify needs and to
detect gaps in service within a system. We began by
reviewing results of needs assessments conducted by several
agencies regarding the relevance of trauma within their
service system and the need for TIC. These needs
Trauma-Informed Care in Homelessness The Open Health Services and Policy Journal, 2010, Volume 3 83
Table 1. Principles of Trauma-Informed Care
Example Definitions of Trauma-Informed Care
Common Principles Across
Definitions
Community
Connections: Five
Guiding Principles for
Trauma-Informed
Services [12]
NASMHPD*: Criteria
for Building a Trauma-
Informed Mental
Health Service System
NCTSN**:
Principles of
Trauma-Informed
Care for Children
NCFH***:
Operating
Principles for
Trauma-
Informed
Organizational
Self-
Assessment
WCDVS****:
Trauma-Informed
or Trauma-
Denied: Principles
& Implementation
of Trauma-
Informed Services
for Women [14].
Consensus-Based Principles
Across Definitions
Theory-Based Expert Trauma Panel Experts
Theory-Based
Research-based
1. Trauma
Awareness
a. Program
philosophy and
mission
Trauma function/ focus,
trauma policy or
position, financing for
best practices, trauma-
informed services,
clinical practice
guidelines for people
with trauma histories,
trauma-informed disaster
planning, systems
integration, research &
data on trauma &
evidence-based & best-
practice treatment
models, access to
evidence-based & best-
practice trauma treatment
Tra
uma
awareness;
basic
understanding
of trauma &
triggers;
includes staff
training &
supervision,
educating
consumers
about trauma
Recognize the
impact of trauma on
development and
coping
b. St
aff
education,
training, and
consultation
Wo
rkforce orientation,
training, support,
competencies and job
standards related to
trauma; promote
education of
professionals in trauma
E
mphasize trauma
recovery as a
primary goal
c.
Practices
Trauma screening and
assessment; Trauma-
specific services,
including evidence-based
and emerging best-
practice treatment
models
Integration
(symptoms
such as
adaptive
coping,
integrating
services,
trauma-specific
services)
d. Recognition of
vicarious trauma
and staff self-
care
2. Safety
a. Physical and
emotional safety
Safety (physical and
emotional)
M
aintaining clear
and consistent
boundaries
Safety, basic
needs,
consistency,
and
predictability
Create an
atmosphere of
safety, respect, and
acceptance
b. Relationships:
authentic,
respectful, clear
boundaries
Trustworthiness (clear
tasks, consistent
practices, staff-consumer
boundaries)
[
see Delivering
services below]
Engagement:
respectful
nonjudgmental
relationships,
clear
boundaries
Utilize a relational
collaboration model.
Growth is fostered
by mutual,
respectful, authentic
relationships
c. Avoid
retraumatization
Procedures avoid
retraumatization and
reduce impacts of trauma
Minimize
retraumatization
84 The Open Health Services and Policy Journal, 2010, Volume 3 Hopper et al.
assessments were generally designed as a first step, prior to
initiating a more formal organizational self-assessment or to
beginning programmatic shifts. Several findings emerged
from a review of these needs assessments:
• Providers feel that they need to be better informed
about trauma and violence [17, 18]. Directors and staff
within state domestic violence coalitions reported that
many shelters are unprepared to deal with the complex
needs of the women they serve, many of whom have
few resources and have been victimized as children and
as adults. Domestic violence advocates reported an
increasing awareness of the need for services appropriate
for women with mental health issues, substance abuse
problems, and histories of abuse. They also expressed a
need for guidance and resources in improving their
responses to survivors of domestic violence who have
experienced multiple abuses throughout their lives [18].
A multi-site program implementing trauma-informed
services found that prior to implementation, sites had
little knowledge about trauma, how to facilitate
recovery, or how services might help or retraumatize
survivors [19].
• Many providers do not have systematic ways of
assessing for trauma-related issues. In a study
examining PTSD screening and referral practices in VA
addiction treatment programs, they found that although
one-half to two-thirds of clinicians did routinely screen
for trauma exposure and posttraumatic stress symptoms,
assessments were generally not conducted system-
atically and did not utilize validated measures [20].
• Consumers want services that are empowering.
Qualitative research has suggested that homeless
individuals and families need and want trauma-informed
services, including desire for autonomy, prevention of
further victimization, and assistance in restoring their
devalued sense of identity [21]. A provider guidebook,
written from a consumer perspective, notes the need
for accessible and effective programs for trauma
survivors [22].
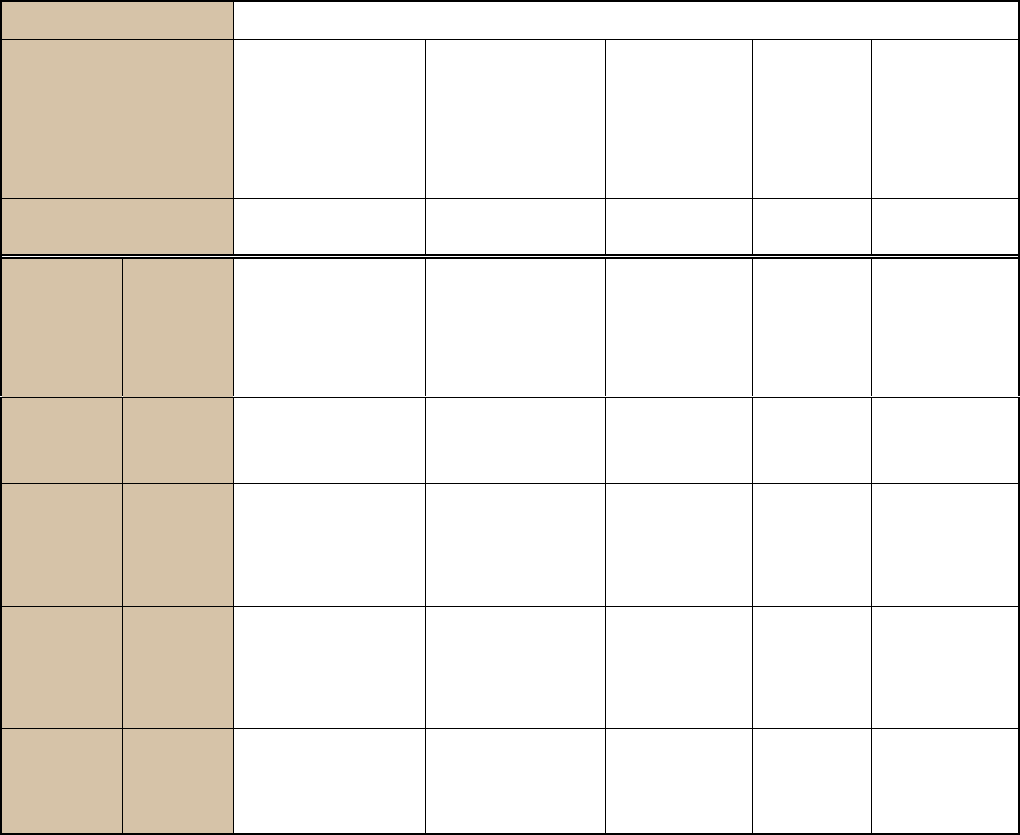
(Table 1) contd…..
Example Definitions of Trauma-Informed Care
Common Principles Across
Definitions
Community Connections:
Five Guiding Principles
for Trauma-Informed
Services [12]
NASMHPD*: Criteria
for Building a Trauma-
Informed Mental
Health Service System
NCTSN**:
Principles of
Trauma-Informed
Care for Children
NCFH***:
Operating
Principles for
Trauma-
Informed
Organizational
Self-
Assessment
WCDVS****:
Trauma-Informed
or Trauma-
Denied: Principles
& Implementation
of Trauma-
Informed Services
for Women [14].
Consensus-Based Principles
Across Definitions
Theory-Based Expert Trauma Panel Experts
Theory-Based
Research-based
d. Acceptance
of and respect
for diversity
Trau
ma policies and
services that respect
culture, race, ethnicity,
gender, age, sexual
orientation, disability,
and socio-economic
status
Delivering services
in a nonjudgmental
and respectful
manner
Cultural
competence
Work towards
cultural competence,
understand
contextual factors
3. Choice &
Empowerment
a. Choice and
control
Choice: maximize
consumer choice and
control
Consumer/Trauma
Survivor/ Recovering
person involvement and
trauma-informed rights
Maximizing choice
and control for
participants
Consumer
control, choice
and autonomy
Underscore
consumers’ choice
and control over
recovery
b.
Emp
owermen
t model
Empowerment: prioritize
consumer empowerment,
skill-building, and growth
Avoidi
ng
provocation and
power assertion
Open
communication:
provide
information
openly to
consumers
Use an
empowerment
model
c. Consumers
involved in
service
development
and
evaluation
Collaboration: maximize
collaboration and sharing
of power between staff and
consumers
Sharing power in
the running of
shelter activities
Shared power
and governance
Involve consumers
in design and
evaluation of
services
4. Strengths-
based
Focus on
strengths,
resiliency
[see Empowerment above]
Hea
ling,
instilling hope
Highlight
consumers’
strengths,
adaptations, and
resiliencies
* NASMHPD= National Association of State Mental Health Program Directors.
** NCTSN = National Child Traumatic Stress Network.
*** NCFH = National Center on Family Homelessness.
**** WCDVS = Women, Co-Occurring Disorders and Violence Study.
Trauma-Informed Care in Homelessness The Open Health Services and Policy Journal, 2010, Volume 3 85
• Mental health services are an important need for
many homeless families and individuals. In a multi-
site research study on trauma-informed services for
homeless families, researchers examined current service
needs, including families’ need for social capital
(educational or employment-related interventions),
physical health, and mental health/substance use
treatment. Among the families, they found that “mental
health needs were the most prevalent of all the
intervention needs components across sites (62%),” with
many facing multiple challenges, signaling the need for
comprehensive intervention [23].
The results of these needs assessments supported the central
importance of dealing with trauma within homelessness service
settings and the perceived need for TIC.
Trauma-Informed Care within Homelessness Services
Settings: Attitudes, Implementation, and Outcomes
Once the perceived need for trauma services is established,
we can begin to explore the development of a TIC framework
within homelessness service settings. We reviewed available
quantitative, qualitative, and corroborative evidence regarding
trauma-informed services.
Prochaska’s stages of change model [24] highlights the fact
that change is a process for individuals, who progress through
precontemplation, contemplation, action, and maintenance of
change. Similarly, systems change is a multi-step process. Our
review of the literature highlighted three areas of evidence:
attitudes, implementation, and outcomes. “Attitudes” refers to
the beliefs of consumers and providers (at all levels, from
management to front-line workers) of the need for a paradigm
shift, confidence in ability to institute a paradigm shift, and
belief that such a shift will lead to positive outcomes.
“Implementation” coincides with Prochaska’s action stage of
change. It is a process variable, and is concerned with how
changes are made. Implementation requires a clear definition of
what is meant by Trauma-Informed Care, in order to translate
these principles into concrete changes that will be instituted
within the system. Finally, “outcomes” refers to the impact of a
paradigm shift to TIC within homelessness service settings.
Measurable objectives help to assess the efficacy of systems
change. Outcomes may include measurable quantitative
outcomes, such as a decrease in recidivism in homelessness, or
qualitative outcomes, such as self-esteem or satisfaction with
services.
Review of the Evidence: What Do We Know About TIC?
In our review of the evidence for TIC, several salient points
emerged:
1. Attitudes
• Programs attempting to implement TIC have
encountered some concerns and resistance on the
part of providers. Providers may be afraid that
addressing trauma will open a “Pandora’s box” of
reactions. They may lack confidence in their ability to
manage and address trauma reactions and may be
concerned that they will encounter triggers of their own
trauma histories [19]. They may also worry that they
will not have the resources to adequately respond to the
complex needs of survivors.
• Because of these concerns, taking the time to build
“buy
-in” is particularly important. Recognizing the
importance of commitment in organizations, some
programs have developed committee structures
geared towards obtaining “buy-in” from
administration, program staff, and consumers.
Building strong relationships also aided buy-in and
integration of services [19]. After building agency-
wide commitment, programs have found strong
support from staff members for implementing a
trauma-informed model [25].
• Consumers want providers who are empathic and
caring, who provide validation, and who offer
emotional safety—characteristics of trauma-
informed providers. Consumers have emphasized
the benefits of working with trauma-informed
providers. Some have suggested that programs could
benefit from having more trauma services, that
practitioners need to remain patient, and that
consumers themselves need to be invested in actively
addressing their own issues [26]. However, even
within trauma-informed systems, consumers
sometimes struggle to feel empowered within a larger
service system [27].
2. Implementation
• Training is central to implementing TIC. The
majority of programs working to build TIC utilized
staff training to increase awareness of and sensitivity
to trauma-related issues. A large multi-site study of
trauma-informed models found that “training on
trauma for non-trauma providers was the first and
most important step in making services more trauma-
informed” [19].
• Ongoing supervision, consultation, and support
are needed to reinforce trauma-based concepts.
One lesson from WCDVS was the importance of
ongoing supervision and support to ensure that the
environment is trauma-informed and that staff
members practice appropriate self-care. Many
programs also used external trauma consultants and
ongoing training to reinforce knowledge and
commitment to building trauma-informed services
[19].
• Assessment and screening are important aspects of
trauma-informed services. Research documenting
high prevalence rates of trauma among people
experiencing homelessness has led to the conclusion
that screening for trauma is important within
homeless service settings [28]. Although providers
have at times expressed concern that inquiring about
trauma histories will lead to traumatic stress
responses, findings indicate that there are few adverse
reactions to screening and assessment. Instead, most
people benefit from this type of assessment [29].
Several pilot studies show that providers refined their
intake processes to include screening for trauma
exposure [28, 30]. Additionally, screening and
assessment tools should be revised and refined with
consumer and provider feedback [29].

86 The Open Health Services and Policy Journal, 2010, Volume 3 Hopper et al.
• Because homeless individuals often have a
multitude of service needs, comprehensive and
integrated services are essential. Studies have found
that service settings offering integrated counseling—
addressing trauma, mental health, and substance use
issues—had better results than settings that were not
integrated [31].
• Integrating trauma-informed services for children
is
also important. Children of parents who are
dealing with trauma, mental illness, substance abuse,
and/or homelessness may be at greater risk for
adverse outcomes. A number of programs working to
integrate trauma-informed services have also
highlighted the importance of parallel services for
children. In WCDVS, a subset of sites offered
specialized children’s programs, including
assessment, groups, and resource
coordination/advocacy for children to build coping
skills, strengthen interpersonal relationships, and
develop positive identity and self-esteem [32].
• Many factors challenge implementation of
trauma-informed services. Various reports
highlighted the logistical difficulties of systems
change. Change, especially within larger systems, can
be time-consuming and requires a great deal of
commitment across all levels of an organization.
Organizational resistance and stress can be a barrier
to larger systems change [33]. Moses highlighted
challenges to systems change across a number of sites
working to implement integrated, trauma-informed
services for women with co-occurring disorders.
These challenges included philosophical differences
between mental health and substance use treatment
approaches, differences around issues of trauma,
resistance at the service and administrative levels,
limited resources, difficulties in achieving consistent
participation in trauma groups, staff turnover, and the
difficulty of change in general [13].
• Implementing a trauma-informed model can lead
to changes in how an organization functions. In a
program implementing a trauma-informed model,
staff reported a number of changes within their
programs, including increased awareness and
sensitivity about trauma, intake that incorporates
questions about trauma, more freedom and choice
given to consumers regarding their treatment, and
environmental changes that led to increases in safety,
confidentiality, and a more welcoming atmosphere
[30].
• Including consumers in developing and evaluating
trauma-informed services is important. Although
there has not yet been research that examines
differences in services that include or do not include
consumers in program development and evaluation,
current wisdom in the field stresses the importance of
including consumers in all aspects of programming
[34, 35]. This wisdom is consistent with theories on
empowerment, which suggest that survivors should
be given agency in effecting their own outcomes [36].
The WCDVS found that integrating consumers into
the design and evaluation of services had a profound
impact on the systems involved [19], and that
“integral to the… group's personal and professional
growth was the development and expression of their
individual and collective voices” [27].
• Cultural competence is important in developing
TIC. Because trauma may have different meanings in
different cultures, and because traumatic stress may
be expressed differently within different cultural
frameworks, it is important for providers within a
trauma-informed system to work towards developing
cultural and linguistic competence [13].
3. Outcomes
• Trauma-informed service settings, with trauma-
specific services available, have better outcomes
than “treatment as usual” for many symptoms. We
know from a variety of studies [31, 37] and pilot
programs [38] that setting that utilize a trauma-
informed model report a decrease in psychiatric
symptoms and substance use. Some of these programs
have shown an improvement in consumers’ daily
functioning and a decrease in trauma symptoms,
substance use, and mental health symptoms. These
findings suggest that integrating services for trau-
matic stress, substance use, and mental health leads to
better outcomes [16].
• TIC for children lead to better outcomes, such as
better self-esteem, improved relationships, and
increased safety. A subset of programs within
WCDVS examined the impact of a standardized,
trauma-informed intervention for children, consisting
of a clinical assessment, coordination of resources
and advocacy, and a psycho-educational skills-
building group. One year later, children in the
intervention group had more positive self-identity,
increased tools for building healthy relationships, and
improved safety. These changes were particularly
striking for children who had witnessed violence [32,
39].
• Early indications suggest that TIC may have a
positive effect on housing stability. A multi-site
study of TIC for homeless families found that, at 18
months, 88% of participants had either remained in
Section 8 housing or moved to permanent housing
[23]. An outreach and care coordination program that
provided family-focused, integrated, trauma-informed
care to homeless mothers in Massachusetts found that
the program led to increased residential stability [38].
• TIC may lead to a decrease in crisis-based
services. Some studies have found decreases in the
use of intensive services such as hospitalization and
crisis intervention following the implementation of
trauma-informed care [40].
• Trauma-informed, integrated services are cost-
effective. Because trauma-informed integrated
services have improved outcomes but do not cost
more than standard programming, they are judged to
be cost-effective [41].
•
Qua
litative results find that providers report
positive outcomes in their organizations from
Trauma-Informed Care in Homelessness The Open Health Services and Policy Journal, 2010, Volume 3 87
implementing TIC. Providers report greater
collaboration with consumers, enhanced skills, and a
greater sense of self-efficacy among consumers, and
more support from their agencies. Supervisors report
more collaboration within and outside their agencies,
improved staff morale, fewer negative events, and
more effective services [40].
• Qualitative results indicate that consumers
respond well to TIC. Within the D.C. Trauma
Collaboration study, consumers reported an increased
sense of safety, better collaboration with staff, and a
more significant “voice.” Eighty-four % of consumers
rated their overall experience with these trauma-
informed services using the highest rating available
[42]. Survey results suggest that consumers were very
satisfied with trauma-informed changes in service
delivery [25].
These results reinforce the need for TIC, assist in further
defining TIC, clarify the process of implementation, and
suggest the efficacy of TIC for certain outcomes. However,
in our review, we found that various questions were not
addressed by available evidence. These gaps in the available
evidence are important in highlighting the additional work
that remains to be done to implement TIC in homelessness
service settings.
Review of the Evidence: What Do We Not Know About
TIC?
Our review of the literature highlighted several directions
for future exploration:
1. Attitudes
• Although providers and consumers alike generally
pay lip service to the idea of TIC, we do not know
the extent to which their attitude is influenced by
demand. In much of the research to date, providers
and consumers were given brief questionnaires or
were interviewed—in many cases, by the individuals
working to build trauma-informed services. Thus,
there may be a tendency to indicate support of
implementation plans and strategies in the absence of
true commitment.
2. Implementation
• We do not know exactly what constitutes “trauma-
informed care.” Trauma has become a buzz-word
recently, with many agencies and workgroups noting
the importance of becoming “trauma-informed.”
However, definitions of “trauma-informed” and how
these ideas are implemented vary widely. There is
generally a lack of specificity in how agencies are
defining “trauma-informed,” and how this relates to
actual practice.
• We do not have a clear method for measuring the
degree to which a program is trauma-informed.
Because of the lack of definitions and behaviorally-
defined changes signifying trauma-informed services,
there is no consistent basis for identifying whether or
not and to what degrees a program is trauma-
informed.
• We do not know how special populations respond
to trauma-informed homelessness services. Much
of the evidence on trauma-informed homelessness
systems concerns women and children. We know less
about the response of other groups, such as men,
veterans, individuals from ethnic/racial minorities or
other cultures, and lesbian, gay, bisexual and
transgendered (LGBT) individuals.
3. Outcomes
• We do not know whether differences in outcomes
are based on trauma-informed environments,
trauma-specific interventions, or both. Because
many service settings that provide TIC also offer
trauma-specific services, the extent to which each
component contributes to change is difficult for
research studies to determine.
• We do not know whether trauma-informed
services are effective specifically within homeless
services. Although the research in other fields
suggests that trauma-informed services may be
effective for homeless individuals, there have yet to
be any rigorous, quantitative studies exploring
outcomes within homelessness service settings. The
results of the Homeless Families Program, a current
multi-site evaluation of trauma-informed
homelessness services, may begin to shed some light
on this issue.
Our review of the current evidence suggests that TIC is
an i
mportant area for further exploration. Initial feedback
appears to support the assertion that TIC has a positive
impact on both the process and outcome of service provision
within homelessness service settings. However, the review
highlighted as many questions and gaps as it defined results
and conclusions.
Because the implementation of TIC within homelessness
service settings is in its infancy, it is particularly important to
review lessons from the field, including self-assessments and
frameworks that are being developed to guide the paradigm
shift to TIC, as well as feed back from local, regional, and
national programs and initiatives that are implementing TIC.
Lessons from the field highlight clinical insights, new
practice initiatives, and areas in need of further qualitative
and quantitative research.
Corroborative Evidence: Lessons from the Field on
Building TIC in Homelessness Service Systems
When we look to the field for best practices and clinical
wisdom, we find a wealth of information about current
theories, practices, programming, and policy initiatives. This
information tells us that although we do not yet have
substantial outcome-based research supporting the
effectiveness of TIC, there is considerable activity in the
field that is awaiting additional documentation. Many
homeless service systems are beginning to address this
issue—administrators, providers, consultants, and consumers
are working together to transform programs into
environments that offer TIC.
After recognizing the pervasiveness of traumatic stress
among people experiencing homelessness, various programs
are taking steps to become more trauma-informed. We have
88 The Open Health Services and Policy Journal, 2010, Volume 3 Hopper et al.
selected several case examples to describe the ways in which
homeless service settings are striving to become more
trauma-informed. This is not a comprehensive list of trauma-
informed resources and programs. Instead, it is intended to
illustrate various creative ways that programs are
implementing trauma-informed models within homeless
service systems, and some of the tools that are available to
aid this transition.
Selected Promising Models
T
o foster the development of trauma-informed homeless
service settings without reinventing the wheel within each
individual program, innovators have developed frameworks
and models that can serve as guides for implementing TIC.
Various models have been proposed that support
organizational change towards a model of TIC and that guide
trauma-informed service delivery. Some of these models are:
• Attachment, Regulation, and Competency: A
Comprehensive Framework for Intervention with
Complexly Traumatized Youth (ARC) [43]
• Child Adult Relationship Enhancement (CARE)
• A Long Journey Home [44]
• Phoenix Rising [45]
• Sanctuary Model [46]
• Using Trauma Theory to Design Service Systems
[12]
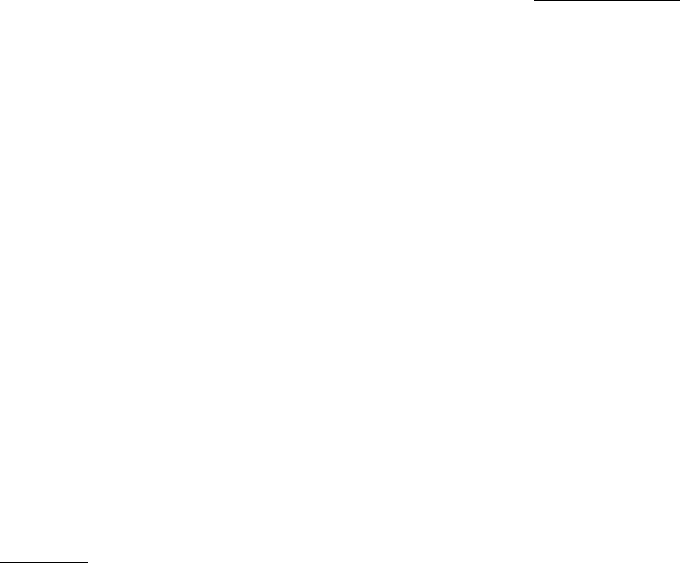
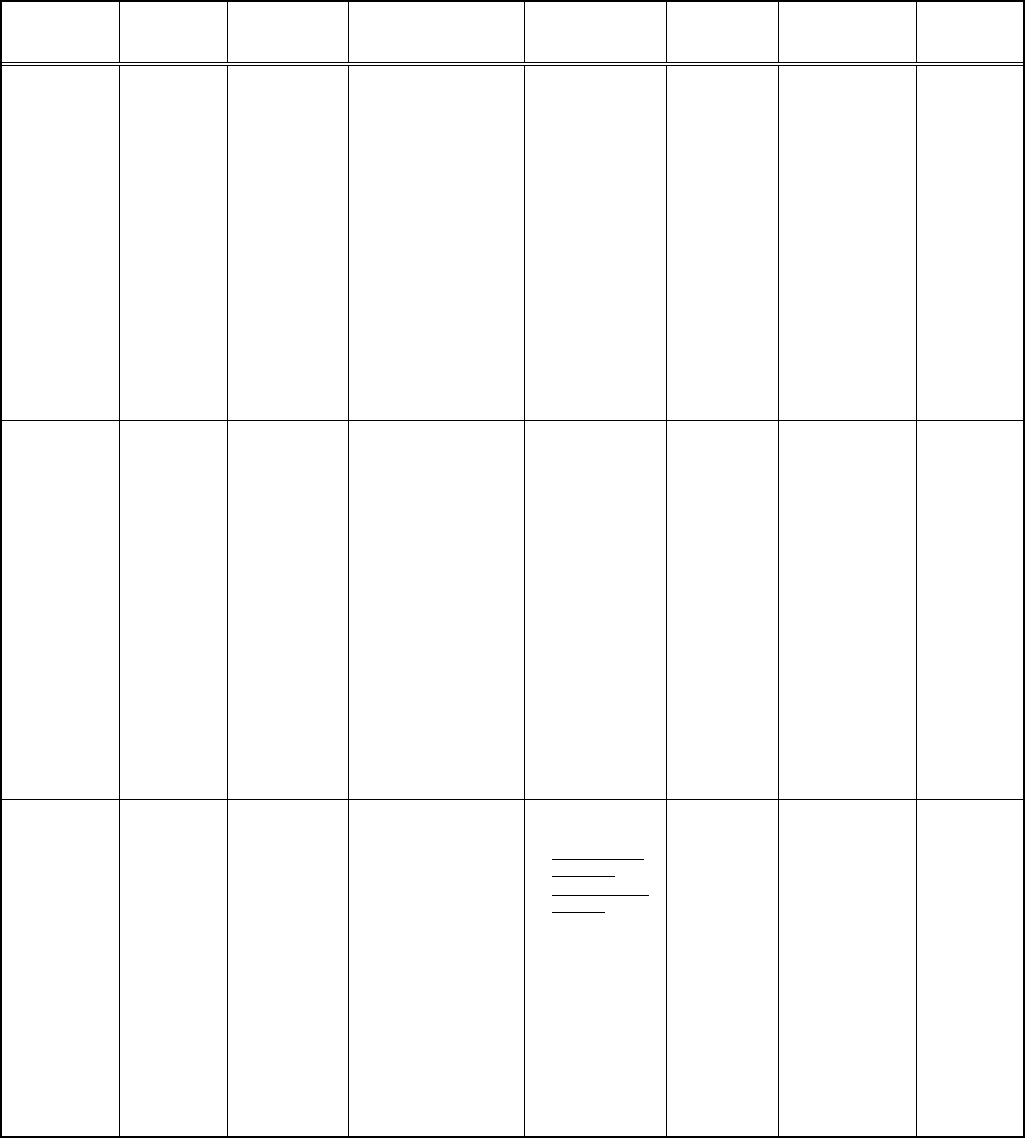
Table 2 describes each of these models, the applications
of the models, and available evidence supporting their
effectiveness. These models of TIC emphasize staff
education, involving consumers, and transforming systems to
be responsive to the needs of trauma survivors. Several
models, including ARC, CARE, and Sanctuary, have an
evidence base (e.g., outcomes-based quantitative research) in
the mental health field (including inpatient and outpatient
settings) and are considered to be promising practices in
trauma-informed care [46]. Others, such as A Long Journey
Home and Phoenix Rising, were developed specifically for
homeless service settings. Most of these models have been
implemented within homeless service settings, and process
and outcome evaluation data are currently being collected.
HOW TRAUMA-INFORMED ARE WE?
ORGANIZATIONAL SELF-ASSESSMENTS
The models described above highlight the need for a
framework that provides the foundation for a paradigm shift
within homelessness service systems. Once a model for TIC
has been identified, an organizational self-assessment can be
utilized as a starting point for systems change.
Self-assessment targets specific areas for change and
indicates how a service delivery model might be adapted to
an organization’s unique needs. As the model is
implemented, a self-assessment is a useful reminder about
important aspects of trauma-informed care that facilitate self-
monitoring and program evaluation. Organizational self-
assessments can also be conducted after implementation of a
paradigm shift in order to evaluate the effectiveness of the
systems change.
Several trauma-informed organizational self-assessments
are currently available or/are in development. They include:
• The Collaboration on Trauma-Surviving Homeless
Children, a partnership between the National Center
on Family Homelessness and the Trauma Center at
Justice Resource Institute (JRI), has developed the
Trauma-Informed Organizational Self-Assessment
for Programs Serving Homeless Families [50] to
help programs assess the degree to which their
services are trauma-informed and to highlight areas
for change. The self-assessment addresses
organizational issues such as delineating program
mission, guidelines, and policies; reviewing services
and policies; establishing a safe and trauma-informed
physical environment; respecting consumer needs and
differences; protecting consumer privacy and
information; encouraging internal and external
community-building; and involving consumers in
program development and evaluation. The instrument
evaluates staff issues, including hiring practices, staff
training and education, and supervision and support.
It also assesses consumer issues, including procedures
for arrival and intake; safety-planning and crisis
prevention; goal setting; and availability of services,
including trauma-specific interventions.
• The Trauma Center at JRI has developed the
Trauma-Informed Facility Assessment [49], a brief
instrument assessing the degree to which an
organization’s physical space is trauma-informed.
This assessment defines several characteristics that
are of primary importance for trauma-informed
organizations, including physical safety, absence of
triggering material, privacy/ confidentiality, and
structure and predictable/consistent response. Other
areas measured by the instrument include
accessibility; organization and hygiene; the ability to
meet the basic needs of consumers and provide links
to resources; the availability of personal/quiet space;
the communication of positive messages; and the
creation of a sense of community, with consumer
ownership of the space and the program.
• Community Connections has developed a Trauma-
Informed Program Self-Assessment Scale and
Planning Protocol [51]. This tool allows
organizations to evaluate the degree to which
program activities and settings are consistent with
five guiding principles: safety, trustworthiness,
choice, collaboration, and empowerment. Six major
domains are evaluated, including: program
procedures and settings; formal services policies;
trauma screening, assessment, and service planning;
administrative support for program-wide trauma-
informed services; staff trauma training and
education; and human-resource practices. Each
domain is evaluated on the basis of review of
program policies, standard program activities, review
of physical space, staff ratings, and consumer ratings.
• As part of a larger study examining integrated
trauma-informed treatment for women with
Trauma-Informed Care in Homelessness The Open Health Services and Policy Journal, 2010, Volume 3 89
Table 2. Models of Trauma-Informed Care
Model Developers Description Key Principles Applications
Research
Evidence
Strengths Limitations
The ARC
Model
(Attachment,
Self-Regulation,
and
Competency): A
Comprehensive
Framework for
Intervention
with Complexly
Traumatized
Youth
Kinniburgh
and
Blaustein [48]
•
•
ARC is a
flexible
framework for
intervention
with
children/famil
ies who have
experienced
complex
trauma. ARC
has been
adapted for
use within
various
milieus.
It has been
applied within
homeless
settings for
runaway and
homeless
youth.
•
•
•
•
10 building blocks,
based on three basic
principles:
Attachment,
Regulation, and
Competency.
Attachment:
Caregiver affect
management,
attunement, consistent
responses, routines
and rituals.
Regulation: Affect
identification,
modulation, and
expression.
Competency:
Executive functions,
self-development &
identity, &
developmental tasks.
Therapeutic
Procedures:
• Psycho-
education;
• Relationship
strengthening;
• Social skills;
• Parent-education
training.
• ARC principles
adapted for use
with homeless
adolescents.
• ARC Agency
Inventory for
homeless/
runaway youth
has been
developed.
• Pilot data:
ARC is
effective in
outpatient
settings.
• Quasi-
experimental
research
studies:
conducted in
outpatient and
milieu settings
in MI, IL, CA,
AL, & MA.
Outcomes:
decreased
trauma
symptoms,
PTSD, and
internalizing/
externalizing
symptoms.
• ARC
concepts-
adapted for
use in
homeless
settings but
not yet been
evaluated.
•
•
•
•
•
Very strong
theoretical basis.
Addresses
developmental
trauma.
Offers a
comprehensive
framework for
milieu change;
provides a model
for trauma-
specific
interventions.
Well-defined,
with an extensive
manual and
comprehensive
training
NCTSN calls it a
"promising
practice"
Collecting
evidence on
effectiveness at
multiple sites.
•
Although
evaluated in
multiple
outpatient
and milieu
settings, it
has yet to
be formally
evaluated in
homeless
settings.
CARE
(Child Adult
Relationship
Enhancement)
Trauma
Treatment
Training
Center
(TTTC).
Revised for
homeless
populations by
NCFH & the
Trauma
Center.
•
•
•
Trauma-
informed
modification
of Parent
Child
Interaction
Therapy
(PCIT).
Skill-based
model for use
in milieu
settings.
Being
modified for
homeless
settings.
CARE guides caregivers
in child-directed and
parent-directed
interactions:
• Caretakers’
competence in
managing child's
problematic
behaviors;
• Caretakers’
competence
reinforcing +
behaviors;
• Reduce parent-child
conflict; and
• Enhance positive
parent-child
interactions.
•
•
•
Trauma
education
component.
Live coaching.
Practice of 3 P
Skills (Praise,
Paraphrase, and
Point-Out
Behavior) to
guide parent-
child
interactions.
•
•
•
CARE is
empirically
informed but
has not yet
been
evaluated.
PCIT, the
foundation
for CARE,
has been
empirically
supported by
numerous
studies.
Piloted in
shelters
•
•
•
Modified PCIT-
Strong
theoretical &
research base
Effective for
building +
caregiver/child
relationships &
building
caregiver
competence.
NCTSN calls it
a promising
practice
•
•
Limited
scope in
terms of
systems
change.
Does not
yet have an
evidence
base within
homelessne
ss.
A Long
Journey Home
Prescott, L.
and NCFH
[44]
A Guide for
Creating
Trauma-
Informed
Services for
Homeless
Mothers and
Children
Offers guidance on:
• Changing the
environment
• Trauma-informed
policies and
procedures
• Trauma-informed
services & support
• Client representation
& staff development
• Training and
supervision
•
Developing
sustainability
• Guide offers
concrete
suggestions for
organizational
shift towards
TIC
• Includes concrete
examples,
exercises, &
suggestions for
staff training.
• In the final
stages of
developme
nt; has not
been
piloted in
homeless
service
settings.
•
•
Practical guide
for making
concrete changes
within systems.
Developed
specifically for
trauma-informed
systems change
within homeless
service settings.
• Still in
developme
nt --does
not yet
have a
research or
practice
evidence
base.
90 The Open Health Services and Policy Journal, 2010, Volume 3 Hopper et al.
co-occurring disorders, the W.E.L.L. Project of the
Institute for Health and Recovery (IHR) developed a
toolkit for developing trauma-informed organizations.
This self-assessment tool, entitled Developing
Trauma-informed Organizations: A Toolkit [52],
includes principles of trauma-informed treatment, a
self-assessment for provider organizations, and an
organizational assessment for non-provider
organizations.
Although these self-assessment tools—like the service
delivery models—are still in development and refinement
stages, they reflect advances towards the development of
TIC.
INNOVATIVE PROGRAMS AND INITIATIVES
UTILIZING TIC
The development of these models and self-assessment
tools has facilitated the progress of a number of innovative
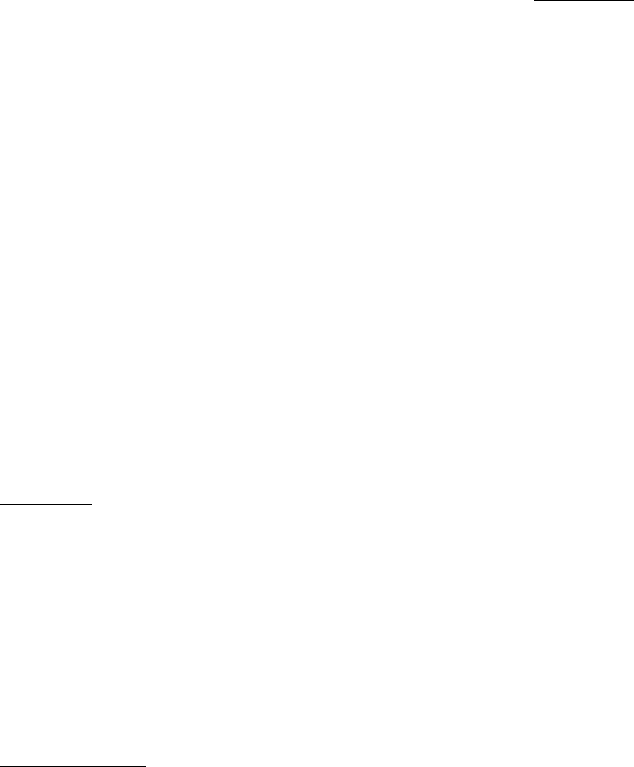
(Table 2) contd…..
Model Developers Description Key Principles Applications
Research
Evidence
Strengths Limitations
Phoenix Rising
Youth on Fire
and the
Trauma
Center at JRI
Phoenix Rising
is an adaptation
of ARC
concepts for use
with homeless
adolescents and
young adults.
Four main components:
• Staff training &
ongoing consultation
• Trauma-informed
milieu changes based
on the Trauma-
Informed Facility
Self-Assessment [49]
• Comprehensive Risk
Counseling and
Services
• Group activities
(expressive art
therapies and
community-building)
Designed for non-
clinical staff in
shelters for
homeless youth.
Offers guidance on:
• Training and
philosophy-shift;
• Self-assessment
• Organizational
and physical
space issues
• Staff issues
• Consumer issues
(skill-building,
development of a
cohesive
environment)
• Being
piloted at a
drop-in
program for
homeless
adolescents
and young
adults in
Cambridge,
MA.
•
•
Practical
guidebook for
concrete
systems
change.
Modification of
a strong
theoretical
model (ARC)
for use at a
drop-in center
for homeless
youth.
•
Manual
under
development
and being
piloted in a
homeless
service
system.
The Sanctuary
Model
Bloom, S. [46]
•
•
Framework
for
intervening
with trauma
survivors and
facilitating
organizational
change.
Originally
developed for
traumatized
adults in
inpatient
units, adapted
for DV
shelters.
• Culture of
nonviolence.
• Emotional
intelligence.
• Inquiry & social
learning.
• Shared governance.
• Open communication.
• Social responsibility.
• Growth and change.
Shared intervention
language: SAGE (Safety,
Affect Management,
Grief, Emancipation) for
adults, SELF (Safety,
Emotions, Loss, Future)
for children.
Concrete tools for
intervention
include:
• Community
meetings
• Red flag reviews
• Psychoeducation
• Self-care
planning
• Safety plans
• Team meetings
• Treatment
planning
conferences
•
•
Program
evaluation
within
inpatient
units:
reduced
PTSD
symptoms
& use of
restraints/
seclusion,
improved
patient
satisfaction,
improved
staff
retention.
Additional
pilot trials
underway.
•
•
•
Theoretical base.
Research
evidence in
multiple settings-
inpatient and
outpatient
NCTSN calls it a
promising
practice
• Although
evaluated
within
multiple
outpatient
and milieu
settings, it
has yet to be
formally
evaluated in
homeless
settings.
Using Trauma
Theory to
Design Service
Systems
Harris and
Fallot [12]
•
Short edited
book
describes
trauma-
informed
systems & the
application of
trauma theory
to systems
change.
Applies
concepts to
various
settings, such
as shelters.
Forms guide
systems
change.
•
•
Systems change
approach.
Self-Assessment and
Planning Protocol
ensures that all levels
of the organization
have an understanding
of trauma, its
sequelae, and the
impact of trauma in
shaping a consumer’s
responses.
•
•
•
•
Book describing
the model:
Using Trauma
Theory to
Design Service
Systems
Trauma-
Informed Self-
Assessment and
Planning
Protocol.
Trauma-
Informed Self-
Assessment
Scale
Implementation
Form.
•
•
Piloted in
DC, ME, &
CT. Most
pilot projects
within
mental health
& substance
abuse
settings.
Initial pilot
project data:
support for
this model
from
organizations
, staff, and
consumers.
•
•
•
Theoretical
base.
Self-
Assessment and
Planning
protocol offers
concrete steps
for
intervention.
Training and
consultation is
available.
•
•
Evidence
base comes
from
unpublished
pilot studies.
Not yet
evidence on
this model
in homeless
service
settings.
Trauma-Informed Care in Homelessness The Open Health Services and Policy Journal, 2010, Volume 3 91
programs that are working to build TIC within homelessness
service systems. We selected various programs that illustrate
lessons from the field with diverse populations experiencing
homelessness.
Trauma-Informed Family Shelters
• The Collaboration on Trauma-Surviving Homeless
Children—a partnership among the National Center
on Family Homelessness, the Trauma Center at
Justice Resource Institute, and other agencies—has
worked with various shelters within the Boston
metropolitan area to build trauma-informed homeless
services. Experts in trauma and homelessness worked
jointly to develop trauma-based training and
consultation targeted specifically to the needs of
homeless families. Trauma training was offered to all
levels of program staff, from administrators to clinical
case managers to family advocates. Staff participated
in regular trauma team meetings that focused on both
trauma-informed organizational change and trauma-
focused case consultation. Trauma-informed
programming was also instituted within shelter
settings. This included community-building activities,
an expressive music program, and self-care activities
for residents. The goal of this program was to
increase the staff’s knowledge of traumatic stress,
their skill level in responding to trauma-related issues,
their self-efficacy about working with individuals and
families who have been traumatized, and their
awareness of issues related to vicarious trauma and
burnout, and self-care. Initial evaluation results
indicated positive outcomes, with high levels of
support for the organizational shift to trauma-
informed programming, increased staff confidence,
fewer resident conflicts, better relationships among
staff and residents, and fewer resident terminations.
Trauma-Informed Domestic Violence Shelters
• The Domes
tic Violence (DV) and Mental Health
Policy Initiative in Chicago is working with the
Department of Public Health, the Mayors Office, and
several domestic violence shelters to create three
“Centers of Excellence” for trauma and domestic
violence. This pilot program will evaluate changes
among organizations, providers, and survivors. The
initiative is also developing a DV-Trauma Core
Curriculum to assist providers in offering more
trauma-informed services within domestic violence
programs.
Trauma-Informed Homeless Outreach Programs
• The Women’s Violence Prevention Project Alliance at
the Friends of the Shattuck shelter in Boston is an
outreach program for homeless men and women that
is working towards becoming more trauma-informed.
This program developed a manual to help providers
and outreach workers build their understanding of
trauma and learn how to respond appropriately to
survivors. The manual also includes a safety-planning
guide for use with individuals who are living on the
streets.
Trauma-Informed Programs for Homeless Youth
• Youth on Fire is a drop-in center for homeless
adolescents and young adults in Cambridge,
Massachusetts. This program utilizes the Phoenix
Rising model, an adaptation of ARC (Attachment,
Self-regulation, and Competency model) for homeless
and at-risk youth. Program staff members have
received trauma training and continue to receive
trauma consultation from the Trauma Center at
Justice Resource Institute. They are working to
modify their environment to become more trauma-
informed. This program also offers trauma-specific
group interventions.
• The Community Trauma Treatment for Runaway and
Homeless Youth is a partnership among several
agencies in the Los Angeles area that provides
outreach and services to homeless youth. This
program has utilized the ARC model to institute a
philosophical shift towards becoming trauma-
informed. They developed an ARC-based
organizational self-assessment in order to target areas
for change within participating agencies. They have
also instituted trauma-informed case conference
meetings in which ARC concepts are used for case
review. Trauma-specific interventions have also been
instituted within this program.
• The Homeless Children’s Network is a consortium of
fifteen homeless and domestic violence programs in
San Francisco, California. This program provides
therapy and case management to homeless children
and their families. Their theoretical framework
considers homelessness to be a traumatic stressor for
children.
Trauma-Informed Treatment Programs for Homeless
People with Co-Occurring Mental Health and Substance
Use Problems
• The Seeking Treatment and Recovery (STAR)
Program in Florida provides treatment for homeless
people who are suffering from co-occurring mental
illness and substance abuse. After determining that
79.5% of the homeless individuals served by their
program acknowledged a history of physical or sexual
abuse, this program began to make changes to
become more trauma-informed. The program
instituted a formal process of screening for trauma
exposure. Based on the high level of trauma exposure
reported by men, they expanded the trauma-specific
services to include treatment for male survivors. The
program also incorporated various training activities
to raise trauma awareness and to build trauma-
informed services [28].
Programs Utilizing a Trauma Framework for Veterans
• Mary E. Walker House is a transitional-living
program for homeless women veterans in Coatesville,
Pennsylvania, that focuses on recovery from trauma
and substance abuse. This program includes a trauma
framework and also offers trauma-specific services.
92 The Open Health Services and Policy Journal, 2010, Volume 3 Hopper et al.
• The Renew program is a V.A. program in Long
Beach, California, which serves both homeless and
non-homeless women veterans who have experienced
military sexual trauma, and often pre-military sexual
trauma.
• New Directions is a V.A. program in Los Angeles,
California, that offers substance abuse and mental
health treatment utilizing a trauma framework. Its
Women’s Program offers trauma counseling, with
100% of clients reporting abuse. The Executive
Director noted, “Most of our clients have experienced
multiple traumas, including physical trauma as a
child, military trauma and years of abuse on the
streets and in prisons. Since veterans are known to
have a higher degree of trauma than the general
public, it would be most cost effective to begin to
treat trauma as the core disability rather than separate
and apart from all other symptoms” [53].
These program examples illustrate the beginning of a
paradigm shift in which homeless services sites are
recognizing the central role of trauma in the lives of
consumers. These programs are being implemented in
diverse settings including family-based shelters, domestic
violence programs, outreach programs, dual diagnosis
programs for homeless individuals, and programs for
homeless youth and veterans. However, this shift is only
beginning. Many programs do not yet recognize the central
role of trauma. Guidance from state and federal initiatives is
likely to facilitate broader awareness of the need for TIC
within behavioral health systems and, more specifically,
within homelessness services settings.
SELECTED STATE AND FEDERAL INITIATIVES TO
ESTABLISH TIC
Over the past ten years, various state and federal policies
have focused on the importance of establishing trauma-
informed services within mental health and substance abuse
settings. In 1998, the National Association of State Mental
Health Program Directors (NASMHPD) issued a position
statement on services and supports for trauma survivors,
recognizing that “the psychological effects of violence and
trauma in our society are pervasive, highly disabling, yet
largely ignored.” The statement articulated a commitment to
address the issue of trauma. The report, Models for
Developing Trauma-Informed Behavioral Health Systems
and Trauma-Specific Services, defined “trauma-informed”
and described programs that have implemented trauma-
informed models on a statewide or local level [54].
NASMHPD also developed a Trauma Services
Implementation Toolkit for State Mental Health Agencies
[42] that describes products being used by various state
agencies to work towards building trauma-informed systems.
Although these policy documents are not directed towards
homeless service systems, they provided momentum in the
social-services fields towards incorporating knowledge of
trauma into service systems.
Regional and national initiatives regarding the need for
TIC within the homelessness field are even more recent.
Within the past ten years, a number of homeless service
organizations and coalitions have begun to emphasize the
importance of addressing the impact of trauma among
individuals experiencing homelessness, and several training
and technical assistance centers have emerged that are
actively promoting trauma-informed homelessness services.
The Homelessness Resource Center (HRC), a
SAMHSA-funded program, provides resources, training, and
technical assistance on issues affecting people who are
homeless. Its mission is to improve the lives of people who
are homeless and have been impacted by trauma, substance
abuse, and mental health issues. One of HRC’s guiding
principles is to foster trauma-informed recovery systems.
Through its website, the HRC disseminates tips, tools, and
knowledge-based products that can be used by programs
interested in implementing trauma-informed care. See
www.homeless.samhsa.gov.
The National Center for Trauma-Informed Care,
funded by SAMHSA’s Center for Mental Health Services
(CMHS), offers educational materials, technical assistance,
and training to social services systems to build an
understanding of the impact of trauma and effective trauma-
based interventions. In collaboration with the Homelessness
Resource Center, the National Center for Trauma-Informed
Care offers trauma-informed training to providers in the Gulf
Coast recovery area. In addition, training in trauma-informed
care has been offered to Projects for Assistance in Transition
from Homelessness (PATH) programs.
The National Child Traumatic Stress Network
(NCTSN), another SAMHSA-supported program, has
focused on the impact of traumatic stress in the lives of
children. The Network has been active in promoting trauma-
informed care, including trauma awareness within homeless
service settings for youth. The Homelessness and Extreme
Poverty Working Group is a branch of NCTSN that devotes
itself to the intersection of trauma, poverty, and
homelessness in children.
The Department of Veterans Affairs offers specialized
services to homeless veterans, and is increasingly addressing
sexual trauma among female veterans. However, the
National Coalition for Homeless Veterans noted that “with
greater numbers of women in combat operations, along with
increased identification of and a greater emphasis on care for
victims of sexual assault and trauma, new and more
comprehensive services are needed.” The Coalition’s 2007
public policy priorities include increasing homeless veterans’
access to comprehensive, high-quality and affordable health
care, including substance abuse and mental health care.
Limitations still exist in the VA’s policy on trauma-informed
care for homeless veterans, particularly around the treatment
of trauma (not necessarily combat-related) among male
veterans.
The work of these initiatives has been integral to raising
awareness of the need for trauma-informed homeless service
systems. However, a large gap still remains between the
recognition of trauma and the implementation of programs
and policies that ensure available and accessible trauma-
informed care for homeless individuals and families. Further
advances in practice, programming, policy, and research are
needed to develop evidence-based, trauma-informed care
within homeless services across the country.
Trauma-Informed Care in Homelessness The Open Health Services and Policy Journal, 2010, Volume 3 93
DISCUSSION
Our review of the current evidence suggested that, while
there are challenges to implementing trauma-informed
services, Trauma-Informed Care appears to be effective. We
can conclude from research in other fields that, with
necessary buy-in, TIC is well-received by consumers and
providers, most likely leads to better outcomes, and does not
cost significantly more than treatment as usual. Despite these
promising findings, this review also highlighted what we do
not yet know about TIC within homelessness services
settings. There is a dearth of research on trauma-informed
approaches specifically within homeless service settings.
Most organizations that are working towards building
trauma-informed homelessness service settings are collecting
minimal or no information for evaluation purposes. The
Homeless Families Program, a large quasi-experimental
study examining trauma-informed services within homeless
services, is an exception.
Initiated by the Substance Abuse and Mental Health
Se
rvices Administration (SAMSHA) in 1999, the Homeless
Families Program is the first large research study to examine
integrated, trauma-informed care for homeless families with
psychiatric disorders, substance use problems, and trauma
histories. Each of the eight sites focuses on helping
consumers understand the connection between their own
trauma histories and their current issues; this education lays
the groundwork for assisting consumers in developing new
coping strategies and working to improve their parenting
skills and relationships. The program also focuses on staff
issues, including team-building, staff support, and self-care.
Although evaluation of the Homeless Families Program
is still in progress, and final results are not yet available,
preliminary findings have identified several factors that seem
to be important for implementing trauma-informed services:
1) the trauma intervention approach should fit into the
overall model and philosophy of the program; 2) programs
should utilize strengths-based approaches in working with
trauma survivors; 3) programs should encourage mutual
respect and trustworthy behavior (e.g., following through on
commitments); 4) programs should avoid punitive
approaches, limiting rules and regulations to those ensuring
safety; 5) staff should be encouraged to have realistic
expectations about the progress that can be expected; 6)
programs should engage survivors in the process of helping
others (e.g., normalizing, empathizing, assisting, allowing
transformative experiences); and 7) programs should
maintain a nonjudgmental approach, while encouraging
personal responsibility and the possibility of making better
choices [55].
Clearly, although initial investigations are promising, the
research to date is inadequate for evaluating the effectiveness
of trauma-informed models within homeless service settings.
Additional quantitative and qualitative research is needed to
further explore trauma-informed practices specifically within
homeless service settings. This research can be used to
establish empirically-based best practices and will be the
springboard for policy that can drive systems change in
programs nationwide. Because the field is only beginning to
generate research-based evidence on trauma-informed
homelessness services, we have looked to the field for best
practices and clinical wisdom in developing and
implementing trauma-informed theories and practices.
RECOMMENDATIONS
This review documents the high rates of traumatic stress
among people who experience homelessness and supports
the need for developing trauma-informed services. While
considerable progress has been made in increasing awareness
of the impact of traumatic stress, the implementation of a
widespread system of trauma-informed homeless services is
in its early stages. Although this review highlights various
innovative practices and programs that have been created in
a wide array of settings for various subgroups of homeless
people, they are relatively limited given the enormous need.
Many program strategies and models are still being
developed and piloted. Preliminary feedback from the
homelessness arena and other service settings suggests that
these approaches may be effective in producing better
outcomes and promoting systems change. However, the
evidence base supporting the effectiveness of these practices
and programs is largely drawn from the corroborative
literature.
The research base supporting the effectiveness of trauma-
informed services within homeless settings is limited. Over
the past decade, trauma-informed services have begun to be
implemented in other fields, including mental health and
substance use programs. With this implementation has come
some robust quantitative and qualitative research.
Quantitative research from these fields indicates that trauma-
informed services are associated with improved outcomes,
such as decreased mental health, trauma-related, and
substance abuse symptoms and behaviors. Qualitative
research from these fields has better described the meaning
of trauma-informed care and has found that its
implementation can be a challenging process, but that it can
lead to systems changes that have positive impacts on both
providers and consumers. Findings from these studies can
inform best practices within the homelessness field.
Even with significant limitations in the research
literature, we have learned important lessons about how we
can best move ahead to make the homelessness service
system more trauma-informed.
Practice
Despite the prevalence of trauma among individuals
experiencing homelessness, many homeless service systems
are not yet adequately addressing this issue. Greater
uniformity and consistency of trauma-informed services for
homeless individuals will aid in our understanding of the
effectiveness of those practices.
Practice recommendations for building trauma-informed
homeless services include the following:
1. Although a number of homeless services settings may
be beginning to implement trauma-informed services,
there is great variability in how these services are
implemented. Utilization of a theory-based model or
framework would help to ensure consistency across
sites and help to begin to build evidence-based
practices.
94 The Open Health Services and Policy Journal, 2010, Volume 3 Hopper et al.
2. Programs should strive to avoid any practices that
may be retraumatizing. This applies to all levels of
the system, including administrative, provider, and
consumer levels.
3. Homeless service systems should implement
universal systematic screening for trauma histories,
using standardized measures.
4. Program intake and evaluation should include an
as
sessment of consumer strengths and resources. This
contributes to the development of a strengths-based
model and supports the further development of
coping resources.
5. Because research has found that integration of
services is a key factor in improving outcomes, it is
recommended that substance abuse, mental health,
and trauma services be integrated.
6. Programs implementing integrated trauma-informed
treatment approaches should also include trauma-
informed services for children, in order to increase
resiliency in children and youth.
7. Because the majority of consumers in homeless
service settings are trauma survivors, additional
trauma-specific services should be made available for
consumers who wish to receive targeted treatment.
8. Building on empowerment-based trauma theories
emphasizing the importance of actively participating
in service programs and rebuilding a sense of control,
programs should support and encourage consumer
involvement. Examples of consumer involvement
include active goal-setting and crisis planning, peer-
led services, leadership roles for consumers, and
involvement in program design, evaluation, and
refinement.
9. All trauma-informed services should be culturally
and linguistically competent.
Programming
Our review of the theory, study, and practice of trauma-
informed services underscored six steps that are essential
when implementing a trauma-informed model, including:
1. Obtaining “buy-in” at multiple levels within the
system
2. Conducting a needs assessment to identify areas for
change
3. Reviewing the organization’s environment,
procedures, and services and revising them to become
more aligned with the principles of trauma-informed
care
4. Providing training on trauma
5. Offering ongoing trauma-based consultation and
supervision
6. Providing access to trauma-specific interventions
These principles and implementation strategies are a
starting point for any program wishing to implement trauma-
informed services.
Beyond offering services that have a trauma-based
framework, programming efforts are needed to establish
agency-wide commitment to building trauma-informed
services. Programming builds continuity among providers to
establish the overall shift in program philosophy necessary
for building trauma-informed services.
1. Homeless programs should integrate trauma
awareness and responsiveness into their program
missions.
2. There is a need to operationalize the principles of
trauma-informed services, and to link these principles
to quantitative, measurable changes that can be
tracked and evaluated.
3. Guidelines should be developed for implementing a
trauma-informed model or framework in homeless
service settings.
4. Programs working for larger systems change towards
a trauma-informed model should start with an
organizational self-assessment in order to identify
strengths and target areas for change.
5. Organizations should institute regular internal and/or
external reviews to assess the degree to which their
programs are trauma-informed.
6. Despite the fact that they work with trauma survivors
on a daily basis, most staff members within homeless
services are not trained about the impact of trauma or
strategies for working with trauma survivors.
Homeless services should implement standardized
training on understanding traumatic stress and
working with trauma survivors. Because these
concepts are complex and cannot be adequately
covered in one training, regular follow-up trainings
should be offered.
7. A consultation model that is ongoing and responsive
to specific needs should be utilized to reinforce
concepts learned in trainings, as well as to help
providers apply what they have learned to actual
situations in their service settings.
8. Regular supervision should be offered in order to
assist staff members in understanding the impact of
trauma in particular situations, and to aid staff in
recognizing and managing their own reactions.
9. Homeless services should design trauma-informed
environments, including attention to issues of
physical space, triggering materials, privacy/
confidentiality, and structure/ predictability.
10. Policies and protocols should be reviewed to ensure
that they are consistent with a trauma-informed model
and are not inadvertently retraumatizing.
11. Homeless service organizations should be aware of
and responsive to issues of job stress, burnout, and
vicarious trauma in providers. Programs need to have
structures in place for prevention of, and early
intervention for, vicarious trauma. In terms of
prevention, it is recommended that organizations
institute policies, programs, or activities that
encourage staff self-care and support.
Trauma-Informed Care in Homelessness The Open Health Services and Policy Journal, 2010, Volume 3 95
12. Consumer involvement is an integral part of a trauma-
informed system. It is recommended that consumers
of homeless services participate as active members in
program development, operation, and evaluation.
Some possibilities for this involvement include: Town
Hall meetings, consumer advisory boards, and peer-
led groups. Prescott [22] offers guidelines for
integrating consumers into trauma-informed
programs.
13. Services and programs should promote cultural
diversity and competency.
Policy
The evidence on trauma-informed services in homeless
settings is limited and there is a lack of clearly defined
principles, definitions, and methods for establishing trauma-
informed services. More research is needed to evaluate the
process of developing trauma-informed services and to
evaluate the effectiveness of trauma-informed services for
homeless individuals. State and federal funding should be
appropriated for examining evidence for trauma-informed
interventions. The National Association of State Mental
Health Program Directors (NASMHPD) has taken a first step
in this direction by recommending that states establish
financing criteria and mechanisms for funding best-practice
trauma treatment models and services. However, these policy
efforts should be expanded to include federal and local
funding, and to include a focus on homeless service settings.
The current review of trauma-informed homeless
services suggests a number of policies whose adoption is
necessary to move the field further:
1. Policies should support homeless services that
employ strategies to prevent trauma exposure,
including the elimination of practices that are
retraumatizing.
2. Policies should support increased capacity for early
detection of trauma within homeless service settings.
3. Mainstream services should be available and
accessible to individuals experiencing homelessness
and should be responsive to the needs of trauma
survivors.
4. Policies should guide the development and offering of
comprehensive, integrated, trauma-informed
treatment within homeless service settings.
5. Policies should prescribe and define consumer
involvement in developing and evaluating homeless
services.
6. Policies should ensure that funding is available to
develop and sustain trauma-informed care.
7. Policies should ensure that services are designed to be
developmentally-appropriate, and culturally and
linguistically competent.
8. Trauma-informed homeless service policies need to
be supported by larger systems guiding services for
homeless individuals and families, including national,
state, and local governmental, community-based
groups, and non-profit organizations. Some of these
systems include: the U.S. Department of Health and
Human Services, the U.S. Department of Veterans
Affairs, the U.S. Departments of Housing and Urban
Development, the U.S. Interagency Council on
Homelessness, state-level councils to end
homelessness, the National Alliance to End
Homelessness, the National Health Care for the
Homeless Council, the National Law Center on
Homelessness and Poverty, the National Center on
Family Homelessness, and the Homelessness
Resource Center.
Research
There is a paucity of research examining the
effectiveness of trauma-informed services for homeless
individuals and families. Most programs that have begun to
institute trauma-informed practices have not tested their
models for effectiveness. This may be due to financial
constraints and to the fact that many programs are focused
on direct service, as opposed to research.
1. Although research on trauma-informed services in the
mental health and substance use fields is promising,
further research is needed on developing trauma-
informed services within homeless service settings.
2. Researchers and providers need to establish a greater
consensus about what constitutes a “trauma-informed
service system.” Clearly defining what is meant by a
“trauma-informed system” will create greater
uniformity in research, increasing the ability to
compare strategies for implementing trauma-informed
systems.
3. Methods to achieve trauma-informed systems also
need to be more clearly established. The conceptual
framework established by a set of guiding principles
should be behaviorally defined within a system. This
allows fidelity measurements, indicating the degree to
which a program is meeting the general standards for
a trauma-informed program. Clearly defining
methods will also lead to the possibility of a
classification system delineating varying levels of
trauma-informed systems.
4. Although a number of models or frameworks for
building trauma-informed services have been
developed, more evidence is needed to evaluate and
refine these approaches. Thus, additional research is
needed to evaluate trauma-informed models within
homeless settings. It is recommended that additional
research within the homelessness arena be conducted
using models such as ARC, CARE, A Long Journey
Home, Sanctuary, and Using Trauma Theory to
Design Service Systems.
5. The corroborative evidence that is available offers a
clear starting point for future research on trauma-
informed homeless services. Additional qualitative
research is needed to more clearly define the process
of offering trauma-informed services, while
quantitative studies should follow after models have
been clearly defined and described. These should
examine the outcomes of trauma-informed
interventions.
96 The Open Health Services and Policy Journal, 2010, Volume 3 Hopper et al.
6. Additional research is needed to distinguish the
relative contribution of trauma-informed care, versus
trauma-specific services. The majority of the research
to date on trauma-informed care has also included
trauma-specific services. While clinically this makes
intuitive sense, research is needed to evaluate what
specific factors are leading to change within these
systems.
7. Additional research is required on the needs of
s
pecial populations who are homeless. For instance,
additional research is needed to determine how
trauma-informed care should be adapted to meet the
unique issues faced by youth, veterans, individuals
from other countries, individuals of different ethnic
backgrounds, and LGBT individuals who are
experiencing homelessness.
Trauma-informed homeless services offer a promising
new area for increasingly effective and sensitive service
approaches for highly vulnerable people. Because many, if
not all, homeless individuals have been exposed to high
levels of traumatic stress, it is essential that homeless service
systems develop sensitivity and responsiveness to post-
trauma responses among the people they serve. More efforts
are needed in terms of practice, programming, policy, and
research to continue to build empirically-based, effective
models of trauma-informed care for people who are
struggling daily to exit homelessness.
ACKNOWLEDGEMENTS
Special thanks to Dawn Jahn-Moses of the National
Center on Family Homelessness, and the team at the Center
for Social Innovation.
CONFLICT OF INTEREST
Authors work within organizations that developed some
of the models reviewed (e.g. organizational assessments,
ARC model, Phoenix Rising).
This document was developed under Contract No.
HHSS280200600029C from the Substance Abuse and
Mental Health Services Administration (SAMHSA), U.S
Department of Health and Human Services (HHS). The
views, policies, and opinions expressed are those of the
authors and do not necessarily reflect those of SAMHSA or
HHS.
APPENDIX 1
Traumatic Stress and Homelessness
“Homelessness deprives individuals of…basic
needs, exposing them to risky, unpredictable
environments. In short, homelessness is more
than the absence of physical shelter, it is a
stress-filled, dehumanizing, dangerous
circumstance in which individuals are at high
risk of being witness to or victims of a wide
range of violent events” [1].
Researchers have documented that the rates of traumatic
stress are extremely high, and may even be normative,
among those experiencing homelessness. Individuals who
are homeless may have been exposed to neglect,
psychological abuse, physical abuse, or sexual abuse during
childhood; community violence; sexual assault; combat-
related traumas; domestic violence; and accidents or
disasters. A literature review found consistent and well-
documented evidence of high levels of multiple forms of
traumatic stress within individuals and families who are
homeless. It is clear that trauma affects people of every
gender, age, race, sexual orientation, and background within
homeless service settings. No one is immune. The following
data highlight this point:
Men
• More than 2/3 of men in a dual-diagnosis treatment
program for homeless people reported a history of
trauma -- either physical or sexual abuse [28].
• More than 1/4 of homeless men were assaulted in the
past year [56].
• Homeless men within substance treatment programs
have a high prevalence of depression, family
dysfunction, trauma, and multiple previous treatment
experiences [57].
• Despite the fact that men comprise the majority of
homeless people and are frequently exposed to
trauma, homeless men are less likely to receive social
services than homeless women [58], with less effort
directed towards understanding the impact of trauma
for this population.
Women/Mothers
• Although many people think of men when they
consider the issue of homelessness, families—
typically single mothers with young children—now
comprise up to 40% of the overall homeless
population [59].
• Trauma is extremely prevalent among homeless
women: over 90% of homeless mothers report having
experienced severe physical or sexual assault during
their lifetimes [60].
• The majority of homeless mothers were abused
during childhood, with nearly 2/3 reporting severe
physical abuse and 42% reporting sexual abuse; 60%
were abused before the age of twelve [2].
• More than 70% of homeless mothers have at least one
childhood risk factor, including: severe physical
abuse, unwanted sexual contact, having a parent who
was mentally ill or who abused substances, running
away for a week or more, or being in foster care [61].
• Homeless mothers are also frequently the victims of
abuse during adulthood, with 61% reporting a history
of domestic violence and 32% acknowledging recent
domestic violence [2].
• Homelessness puts women at risk for assault; being
homeless was associated with more than three times
the risk of sexual assault for women [56].
• Homelessness and victimization are associated with
adverse mental health outcomes: more than 50% of
homeless mothers reported depression, and more than
40% reported posttraumatic stress disorder (PTSD)
Trauma-Informed Care in Homelessness The Open Health Services and Policy Journal, 2010, Volume 3 97
[62], and were three times as likely as housed women
to suffer from PTSD [63].
Children and Youth
• Child abuse is associated with high-risk behaviors in
adolescents, such as truancy and running away, that
may lead to homelessness [64]. Almost 3/4 of girls on
the streets report that they were forced to run away
from violence at home [65].
• Homeless children and youth are at risk for further
victimization, such as repeated abuse, exposure to
violence, and forced prostitution [66].
• 86% of homeless youth report exposure to trauma,
with almost 2/3 reporting exposure to multiple
traumatic events; physical assaults are prevalent for
young men, while sexual/physical abuse is common
among young women [67].
• Homeless children are at increased risk for medical,
emotional, behavioral, and academic problems,
including post-trauma responses, insecure
attachments, and difficulty learning [60, 68, 69].
Elderly
• The elderly make up a relatively lower percentage of
the homeless population, only 2% [70]; however,
elderly homeless persons are more vulnerable to
victimization, have more health problems, and may be
less likely to receive needed social services and
protection from law enforcement [71].
• In 2006, 27% of the homeless victims of violent
crimes were between 50-59 years of age [9].
Veterans
• Veterans are disproportionately represented in the
homeless population, with veterans making up 23%
of all homeless people in the U.S. [72].
• The majority of women in homeless veteran programs
have serious trauma histories, including being
physically harassed, sexually harassed, or raped while
in the military [73].
• One-quarter or more of homeless veterans manifest
symptoms of PTSD; 76% experience alcohol, drug, or
mental health problems [74].
• Trauma and related distress are related to relapse
and rehospitalization of homeless veterans who have
substance abuse problems, particularly for female
veterans [75].
Minorities
• Minorities are over-represented among the homeless
population, with almost half being African-American
[4].
• Families of color also disproportionately experience
trauma [50].
Lesbian, Gay, Bisexual, & Transgendered (LGBT)
Individuals
• 40% of homeless youth identify as LGBT.
• One-third of LGBT youth are assaulted after
disclosing their sexual orientation; 40% to 60% of
homeless youth cited physical abuse as a reason for
leaving home [76].
• Thirty-three percent of transgendered individuals
reported that they had been physically or sexually
assaulted in the past year [56].
These statistics suggest that it is reasonable to assume
that the majority of homeless individuals have been exposed
to traumatic stress. Most people experiencing homelessness
have been victimized one or more times in their lives. For
many people, abuse began during childhood; in fact,
developmental trauma with disrupted attachments may
provide the subtext for the stories of many people’s
pathways towards homelessness [2]. Violence continues into
adulthood for many people, with abuse such as domestic
violence often precipitating homelessness [3-5], and with
homelessness leaving people vulnerable to further
victimization. In fact, homelessness has been suggested to be
a traumatic event in and of it, compounding the
psychological impact of the myriad risk factors often
experienced by people who are homeless [77]. Based on this
assumption, we can conclude that individuals experiencing
homelessness are, by definition, trauma survivors,
demonstrating the urgency of addressing trauma within this
population.
Another reason that it is important to address trauma
within
homelessness service settings is that victimization is
associated with repeated episodes of homelessness. Research
has found that people who experienced repeated
homelessness were more likely than people with a single
episode of homelessness to have been abused, often during
childhood. First-time homeless mothers who experienced
domestic violence were more than three times as likely to
become homeless again [6]. These findings suggest that we
will be unable to solve the issue of homelessness without
addressing the underlying trauma that is so intricately
interwoven with the experience of homelessness.
As can be seen from this description, the relationship
between trauma and homelessness is complex, with
traumatic stress being a possible core factor increasing
vulnerability to homelessness, and with homelessness
leaving individuals more vulnerable to further victimization.
There is also a complex and multi-directional relationship
between trauma, substance abuse, mental illness, and
homelessness. All these factors need to be addressed in
services for homeless men, women, children and youth, the
elderly, minorities, veterans, LGBT individuals, and other
people.
APPENDIX 2
The Impact of Trauma
Traumatic stress can be devastating and long-lasting. To
develop an understanding about how to build trauma-
sensitive services, we need to first clearly understand that the
impact of traumatic stress can be devastating and long-
lasting, interfering with a person’s sense of self, and sense of
safety, leading to feelings of helplessness, terror, and
disempowerment. Traumatic exposure may lead to responses
98 The Open Health Services and Policy Journal, 2010, Volume 3 Hopper et al.
including Posttraumatic Stress Disorder (PTSD) and
Complex Trauma.
Posttraumatic Stress Disorder (PTSD) re
fers to a group
of symptoms that some individuals experience after
overwhelming, frightening, or horrifying life experiences
that exceed their capacity to cope. PTSD includes intrusive
symptoms such as triggered memories or nightmares,
avoidance symptoms such as social withdrawal, constriction,
and emotional numbing, and symptoms of hyperarousal such
as concentration problems, irritability, and constant alertness
for danger.
Exposure to chronic interpersonal trauma such as child
abuse or domestic violence may have an even more
extensive impact on the survivor, sometimes referred to as
“Complex PTSD,” or “Disorders of Extreme Stress, Not
Otherwise Specified” (DES-NOS). Survivors with Complex
PTSD have difficulty regulating their internal states,
including their emotional states and their physiological
reactions. Their emotions sometimes shift rapidly, leaving
them feeling helpless in the face of overwhelming emotion.
Their bodies are easily activated, resulting in anxiety, panic,
or terror. At other times, they have dissociative responses in
which their bodies or emotions shut down and they become
numb. Triggered responses, reactions to reminders of the
trauma, are also common. In Complex PTSD, the traumatic
experiences impact the survivor’s sense of self; survivors
often blame themselves for their abuse, feeling damaged and
ashamed. Individuals who have experienced chronic
interpersonal trauma often have problems sustaining
supportive relationships, such as difficulty trusting others or
problems establishing clear boundaries and setting limits
with others. This increases their vulnerability to
retraumatization, and interferes with the development of
adequate social networks for support in times of crisis.
Individuals with Complex PTSD may have impaired
Table 3. How Common Trauma Reactions May Explain Some “Difficult” Behaviors or Reactions Within Homeless Service
Settings
"Difficult" Behaviors or Reactions within Homeless Service Settings Common Trauma Reactions
Has difficulty getting motivated to get job training, pursue education, locate a job, or find housing Depression and diminished interest in everyday activities
Complains that the setting is not comfortable or not safe, appears tired and poorly rested. Is up
roaming around at night.
Nightmares and insomnia
Perceives others as being abusive, loses touch with current-day reality and feels like the trauma is
happening over again
Flashbacks, triggered responses
Avoids meetings with counselors or other support staff, emotionally shuts down when faced with
traumatic reminders
Avoidance of traumatic memories or reminders
Isolates within the shelter, stays away from other residents and staff Feeling detached from others
Lacks awareness of emotional responses, does not emotionally respond to others Emotional numbing or restricted range of feelings
Is alert for signs of danger, appears to be tense and nervous Hyper-alertness or hypervigilance
Has interpersonal conflicts within the shelter, appears agitated Irritability, restlessness, outbursts of anger or rage
Has difficulty keeping up in educational settings or job training programs Difficulty concentrating or remembering
Becomes agitated within the shelter. Is triggered by rules and consequences. Has difficulty setting
limits with children.
Feeling unsafe, helpless, and out of control
Has difficulty following rules and guidelines within the shelter or in other settings. Is triggered
when dealing with authorities. Will not accept help from others.
Increased need for control
Feels emotionally "out of control." Staff and other residents become frustrated by not being able to
predict how he or she will respond emotionally
Affect dysregulation (emotional swings – like crying and
then laughing)
Seems spacey or "out of it." Has difficulty
Is not responsive to external situations.
remembering whether or not they have done something.
Dissociation
Complains of aches and pains like headaches, stomachaches, backaches. Becomes ill frequently. Psychosomatic symptoms, impaired immune system
Cuts off from family, friends, and other sources of support Feelings of shame and self-blame
Has difficulty trusting staff members; feels
the service setting.
targeted by others. Does not form close relationships in
Difficulty trusting and/or feelings of betrayal
Complains that the system is unfair, that they are being targeted or unfairly blamed Loss of a sense of order or fairness in the world
Puts less effort
assistance
into trying--does not follow through on appointments, does not respond to
Learned helplessness
Invades others' personal space or lacks awareness of when others are invading their personal space
Boundary issues
Has ongoing substance abuse problems Use of alcohol or drugs to manage emotional responses
Remains in an abusive relationship or is victimized again and again Revictimization (impaired ability to identify danger signs)
Trauma-Informed Care in Homelessness The Open Health Services and Policy Journal, 2010, Volume 3 99
immune system functioning and may experience poor
physical health. They often have difficulty maintaining
attention and concentration and may have memory problems.
Their belief systems about the world are also altered and
they often feel unsafe [78-80].
In describing the link between trauma exposure and
homelessness, Browne [2] wrote, “it seems probable that, for
some homeless women, the effects of early violence or
molestation by intimates decreased their supportive networks
and increased their risk of becoming homeless later in life.”
Thus, exposure to traumatic stress may increase people’s
vulnerability to becoming homeless in certain situations, and
conversely, traumatic stress reactions may make it more
difficult to cope with the stresses inherent in being homeless.
Homeless service providers who lack a basic knowledge
of trauma will not have a context for understanding trauma-
based reactions. Table 3 illustrates behaviors sometimes seen
in homeless service settings that can be confusing or
frustrating for providers or other consumers; column two of
the chart demonstrates how each of these behaviors may be
explained in the context of common reactions to traumatic
stress. This chart highlights the need for understanding
trauma within homeless service settings.
REFERENCES
[1] Fitzpatrick KM, LaGory ME, Ritchey FJ. Dangerous places: Exposure
to violence and its mental health consequences for the homeless. Am J
Orthopsychiatry 1999; 69: 438-47.
[2] Browne A. Family violence and homelessness: The relevance of trauma
histories in the lives of homeless women. Am J Orthopsychiatry 1993;
63: 370.
[3] National Law Center on Homelessness and Poverty. Some facts on
homelessness, housing, and violence against women 2006.
[4] US Conference of Mayors. Hunger and homelessness survey: A status
report on hunger and homelessness in America's cities 2005.
[5] Zorza J. Women battering: a major cause of homelessness. Clgh Rev
1991; 25: 412-29.
[6] Bassuk EL, Perloff JN, Dawson R. Multiply homeless families: The
insidious impact of violence. Hous Policy Debates 2001; 12: 299-320.
[7] Fischer PJ, Breakey WR. The Epidemiology of Alcohol, Drug, and
Mental-Disorders among Homeless Persons. Am Psychol 1991; 46:
1115-28.
[8] Jainchill N, Hawke J, Yagelka J. Gender, psychopathology, and
patterns of homelessness among clients in shelter-based TCs. Am J
Drug Alcohol Abuse 2000; 26: 553-67.
[9] National Coalition for the Homeless. Hate, violence, and death on Main
Street USA: a report on hate crimes and violence against people
experiencing homelessness 2006.
[10] SAMHSA's National Mental Health Information Center. Homelessness
2007.
[11] Goodman LA, Dutton MA, Harris M. Episodically homeless women
with serious mental-illness - prevalence of physical and sexual assault.
Am J Orthopsychiatry 1995; 65: 468-78.
[12] Harris M, Fallot RD. New directions for mental health services: Using
trauma theory to design service systems. San Francisco: Jossey-Bass
2001.
[13] Moses DJ, Reed BG, Mazelis R. Creating trauma services for women
with co-occurring disorders: experiences from the SAMHSA women
with alcohol, drug abuse, and mental health disorders who have
histories of violence study. Delmar, NY: Policy Research Associates,
Inc. 2003.
[14] Elliott DE, Bjelajac P, Fallor RD. Trauma-informed or trauma-denied:
Principles and implementation of trauma-informed services for women.
J Commun Psychol 2005; 33: 461-77.
[15] Olivet J, Bassuk E. Evidence-based practices in homeless services: An
issue brief. Rockville: Center for Mental Health Services 2007.
[16] Morrissey JP, Jackson EW, Ellis AR. Twelve-month outcomes of
trauma-informed interventions for women with co-occurring disorders.
Psychiatr Serv 2005; 56: 1213-22.
[17] Stainbrook KA, Hornik J. Similarities in the characteristics and needs of
women with children in homeless family and domestic violence
shelters. Fam Soc 2006; 87: 53-62.
[18] Warshaw C, Moroney G. Mental health and domestic violence:
Collaborative initiatives, service models, and curricula. Chicago:
Domestic Violence and Mental Health Policy Initiative 2002.
[19] Moses DJ, Huntington N, D'Ambrosio B. Developing integrated
services for women with co-occurring disorders and trauma histories:
Lessons from the SAMHSA women with alcohol, drug abuse, and
mental health disorders who have histories of violence study. Delmar,
NY: Policy Research Associates, Inc. 2004.
[20] Young HE, Rosen CS, Finney JW. A survey of PTSD screening and
referral practices in VA addiction treatment programs. J Subst Abuse
Treat 2005; 28: 313-9.
[21] Padgett DK, Hawkins LR, Abrams C. In their own words: Trauma and
substance abuse in the lives of formerly homeless women with serious
mental illness. Am J Orthopsychiatry 2006; 76: 461-7.
[22] Prescott L. Consumer/survivor/recovering women: A guide for
partnerships in collaboration. Delmar, NY: Policy Research Associates,
Inc. 2001.
[23] Rog DJ, Holupka CS, Mccombsthornton KL. Implementation of the
Homeless Families Program.1. Service Models and Preliminary
Outcomes. Am J Orthopsychiatry 1995; 65: 502-13.
[24] Prochaska JO, DiClemente CC. Stages and process of self-change of
smoking: Toward an integrative model of change. J Consult Clin
Psychol 1983; 51: 390-5.
[25] Community Connections. Final report: Trauma-informed pilot project
at the Rumford (Maine) unit of tri-county mental health services 2003.
[26] Veysey B, Heckman K, Mazelis R. It's my time to live: Journeys to
healing and recovery. Rockville, MD: Substance Abuse and Mental
Helalth Services Administration 2007.
[27] Mockus S, Cinq Mars L, Guazzo Ovard D. Developing
consumer/survivor/recovering voice and its impact on services and
outreach: Our experiences with the SAMHSA women, co-occurring
disorders and violence study. J Commun Psychol 2005; 33: 513-25.
[28] Christensen RC, Hodgkins CC, Garces LK. Homeless, mentally ill and
addicted: The need for abuse and trauma services. J Health Care Poor
Underserved 2005; 16: 615-21.
[29] McHugo GJ, Caspi Y, Kammerer N. The assessment of trauma history
in women with co-occurring substance abuse and mental disorders and
a history of interpersonal violence. J Behav Health Serv Res 2005; 32:
113-27.
[30] Marra JV. Final evaluation report: Evaluation of the trauma center of
excellence initiative. Unpublished program evaluation. Storrs, CT:
University of Connecticut Department of Psychology and the CT
Department of Mental Health and Addiction Services Research
Division 2006.
[31] Cocozza JJ, Jackson EW, Hennigan K. Outcomes for women with co-
occurring disorders and trauma: Program-level effects. J Subst Abuse
Treat 2005; 28: 109-19.
[32] Finkelstein N, Rechberger E, Russell LA. Building resilience in
children of mothers who have co-occurring disorders and histories of
violence: Intervention model and implementation issues. J Behav
Health Serv Res 2005; 32: 141-54.
[33] Bloom S. Organizational stress as a barrier to trauma-sensitive change
and system transformation. Alexaandria, VA: National Technical
Assistance Center for State Mental Health Planning Pulications and
Reports 2006.
[34] McCabe S, Unzicker RE. Changing roles of consumer/survivors in
mature mental health systems. New Dir Ment Health Serv 1995; 66: 61-
73.
[35] National Association of State Mental Health Program Directors.
Position statement on services and supports to trauma survivors 1998.
[36] Zimmerman MA. Toward a theory of learned hopefulness - a structural
model analysis of participation and empowerment. J Res Pers 1990; 24:
71-86.
[37] Morrissey JP, Ellis AR, Gatz M. Outcomes for women with co-
occurring disorders and trauma: Program and person-level effects. J
Subst Abuse Treat 2005; 28: 121-33.
[38] Kammerer N. Project RISE evaluation report. Unpublished program
evaluation report. Boston, MA: Heatlh and Addictions Research, Inc.
and Health Institute for Recovery n.d.
[39] Noether CD, Brown V, Finkelstein N. Promoting resiliency in children
of mothers with co-occurring disorders and histories of trauma: Impact
of a skills-based intervention program on child outcomes. J Commun
Psychol 2007; 35: 823-43.

100 The Open Health Services and Policy Journal, 2010, Volume 3 Hopper et al.
[40] Community Connections. Trauma and abuse in the loves of homeless
men and women. Online PowerPoint presentation. Washington, DC
2002. Available from: http:/www.pathprogram.samhsa.gov/ppt/
Trauma_and_Homelessness.ppt
[41] Domino ME, Morrissey JP, Chung S, Huntington N, Larson MJ,
Russell LA. Service use and costs for women with co-occurring mental
and substance use disorders and a history of violence. Psychiatr Serv
2005; 56: 1223-32.
[42] Jennings A. The damaging consequences of violence and trauma: facts,
discussion points, and recommendations for the behavioral health
system. Alexandria, VA: National Association of State Mental Health
Program Directors, National Technical Assistance Center for State
Mental Health Plannin 2004.
[43] Kinniburgh KJ, Blaustein M, Spinazzola J. Attachment, self-regulation,
and competency. Psychiatr Ann 2005; 35: 424-430.
[44] Prescott L, Soares P, Konnath K, Bassuk E. A long journey home: a
guide for creating trauma-informed services for homeless mothers and
children. Rockville, MD: Center for Mental Health Services, Substance
Abuse and Mental Health Services Administration 2007.
[45] Youth on Fire, Trauma Center at JRI. Phoenix rising: a trauma-
informed approach to HIV/substance use/hepatitis prevention for
homeless and street-involved youth. 2007.
[46] Bloom S. Creating sanctuary: Toward the evolution of sane societies.
New York: Routledge 1997.
[47] National Child Traumatic Stress Network. National child traumatic
stress network empirically supported treatments and promising
practices 2007.
[48] Kinniburgh K, Blaustein M. ARC: Attachment, regulation, &
competency. A comprehensive framework for intervention with
complexly traumatized youth. Brookline, MA: The Trauma Center at
Justice Resource Institute 2005.
[49] Hopper E, Spinazzola J. Trauma-informed facility assessment.
Brookline, MA: The Trauma Center at Justice Resource Institute 2006.
[50] Guarino K, Soares P, Konnath K. Trauma-informed organizational self-
assessment for programs serving families experiencing homelessness.
Rockville, MD: Center for Mental Health Services, Substance Abuse
and Mental Health Services Administration 2007.
[51] Fallot RD, Harris M. Trauma-informed services: a self-assessment and
planning protocol. Community Connections 2002.
[52] Institute for Health and Recovery. Developing trauma-informed
organizations: a toolkit 2002.
[53] Reinis T. New direction: 15 years of service to veterans. Testimony of
Toni Reinis 2007.
[54] Jennings A. Models for developing trauma-informed behavioral health
systems and trauma-specific services. Alexandria, VA: National
Association of State Mental Health Program Directors, National
Technical Assistance Center for State Mental Health Planning 2004.
[55] SAMHSA Homeless Families Coordinating Center. Trauma
interventions for homeless families - Innovative features and common
themes 2005.
[56] Kushel MB, Evans JL, Perry S, Robertson MJ, Moss AR. No door to
lock - Victimization among homeless and marginally housed persons.
Arch Intern Med 2003; 163: 2492-9.
[57] Kim M, Roberts A. Exploring trauma among homeless men in
treatment for substance abuse: a qualitative approach. J Soc Work Pract
Addict 2004; 4: 21-32.
[58] Calsyn RJ, Morse G. Homeless men and women: Commonalities and a
service gap. Am J Commun Psychol 1990; 18: 597-608.
[59] Guarino K, Rubin L, Bassuk E. Trauma in the lives of homeless
families. In: Carll EK, Ed. Trauma psychology: Issues in violence,
disaster, health and illness. Westport, CT, Praeger Publishers 2007; pp.
231-58.
[60] Bassuk EL, Weinreb L. The characteristics and needs of sheltered
homeless and low-income housed mothers. JAMA 1996; 276: 640.
[61] Rog DJ, Mccombsthornton KL, Gilbertmongelli AM. Implementation
of the Homeless Families Program. 2. Characteristics, strengths, and
needs of participant families. Am J Orthopsychiatry 1995; 65: 514-28.
[62] Weinreb L, Buckner JC, Williams V. A comparison of homeless
mothers in Worcester, MA: 1993 vs 2003. Am J Public Health 2006;
96: 1444-8.
[63] Bassuk EL, Buckner JC, Perloff J. Prevalence of mental health and
substance abuse disorders among homeless and low-income housed
mothers. Am J Psychiatry 1998; 155: 1561-4.
[64] Briere JN. Child abuse trauma. Newbury Park, CA: Sage Publications
1992.
[65] Chesney-Lind M, Sheldon RG. Girls, delinquency, and juvenile justice.
Belmont, CA: Wadsworth 1998.
[66] Whitbeck LB, Hoyt DR, Yoder KA. A risk-amplification model of
victimization and depressive symptoms among runaway and homeless
adolescents. Am J Commun Psychol 1999; 27: 273-96.
[67] Gwadz MV, Nish D, Leonard NR. Gender differences in traumatic
events and rates of post-traumatic stress disorder among homeless
youth. J Adolesc 2007; 30: 117-29.
[68] Buckner JC, Beardslee WR, Bassuk EL. Exposure to violence and low-
income children's mental health: Direct, moderated, and mediated
relations. Am J Orthopsychiatry 2004; 74: 413-23.
[69] Cowal K, Shinn M, Weitzman BC. Mother-child separations among
homeless and housed families receiving public assistance in New York
City. Am J Commun Psychol 2002; 30: 711.
[70] US Department of Housing and Urban Development. Ann homeless
assessment report to Congress 2007.
[71] National Coalition for the Homeless. Homelessness among elderly
persons. NCH Fact Sheet #15 2007.
[72] National Coalition for the Homeless. Homeless Veterans. NCH Fact
Sheet #14 2007.
[73] National Coalition for Homeless Veterans. Background and statistics:
Most often asked questions concerning homeless veterans 2005.
[74] McMurray-Avila M. Homeless veterans and health care: a guide for
providers. Nashville: Health Care for the Homeless Council 2001.
[75] Benda BB. Survival analyses of social support and trauma among
homeless male and female veterans who abuse substances. Am J
Orthopsychiatry 2006; 76: 70-79.
[76] Ray N. Lesbian, gay, bisexual and transgender: an epidemic of
homelessness 2006.
[77] Goodman L, Saxe L, Harvey M. Homelessness as psychological trauma
- broadening perspectives. Am Psychol 1991; 46: 1219-25.
[78] Luxenburg T, Spinazzola J, Hidalgo J. Complex trauma and disorders
of extreme stress (DESNOS) diagnosis, part II: Treatment. Dir
Psychiatry 2001; 21: 395-415.
[79] Luxenburg T, Spinazzola J, van der Kolk BA. Complex trauma and
disorders of extreme stress (DESNOS) diagnosis, part I: Assessment.
Dir Psychiatry 2001; 21: 373-93.
[80] van der Kolk BA, McFarlane AC, Weisaeth L. Traumatic stress. New
York: Guilford Press 1996.
Received: August 20, 2009 Revised: September 20, 2009 Accepted: September 28, 2009
© Hopper et al.;
Licensee Bentham Open.
This is an open access article licensed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-
nc/3.0/)/ which permits unrestricted, non-commercial use, distribution and reproduction in any medium, provided the work is properly cited.
